Hyperkalemia: What It Is, Why It Matters, and How Medications Can Trigger It
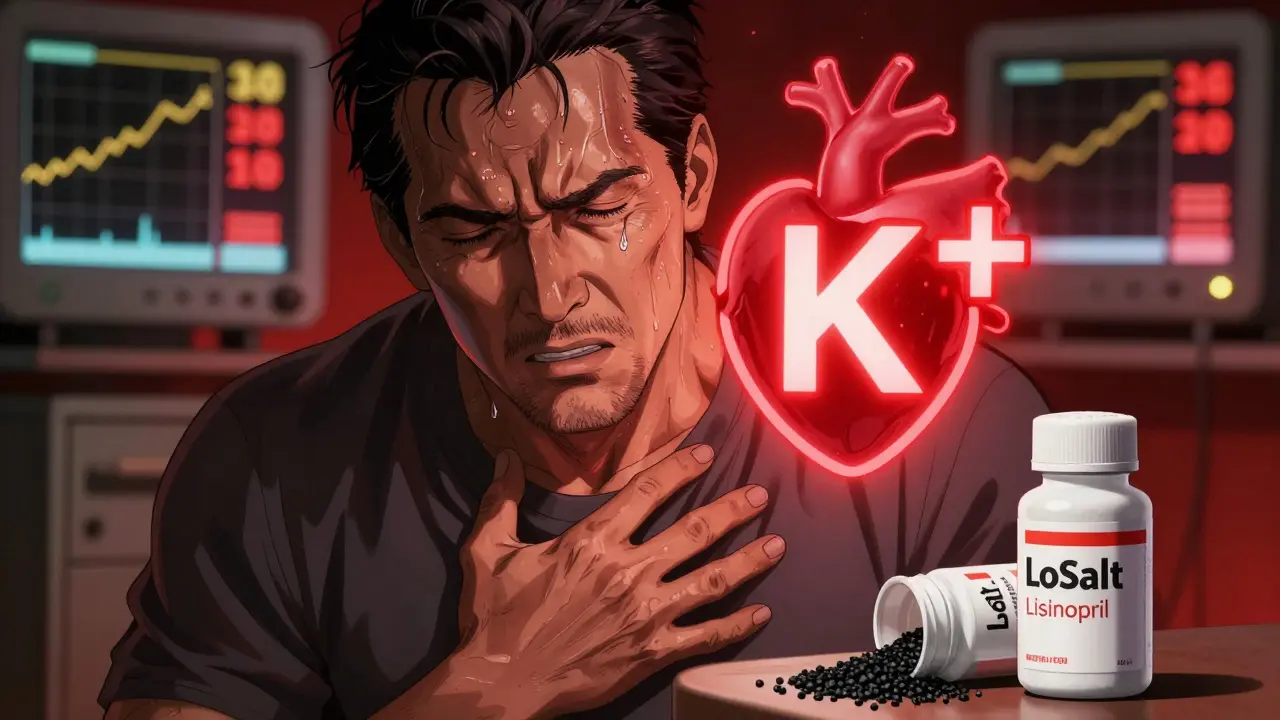
When your blood has too much hyperkalemia, a condition where potassium levels in the blood rise above safe limits. Also known as high potassium, it doesn’t always cause symptoms—but when it does, it can stop your heart. Potassium is essential for muscle and nerve function, especially your heartbeat. But too much of it, even just a little, throws off your heart’s rhythm. This isn’t just a lab number—it’s a silent threat, especially if you have kidney disease, diabetes, or take certain meds.
Many of the drugs you might be taking for common conditions can push potassium up. diuretics, medications used to remove excess fluid from the body. Also known as water pills, they’re often prescribed for high blood pressure or heart failure. But not all diuretics are the same. Some, like spironolactone, actually keep potassium in your body. That’s helpful in some cases, but dangerous if your kidneys can’t clear the extra. Other common culprits include ACE inhibitors, ARBs, and NSAIDs. If you’re on any of these, your doctor should check your potassium regularly. Most people never know their levels are rising until they feel dizzy, weak, or get an abnormal EKG.
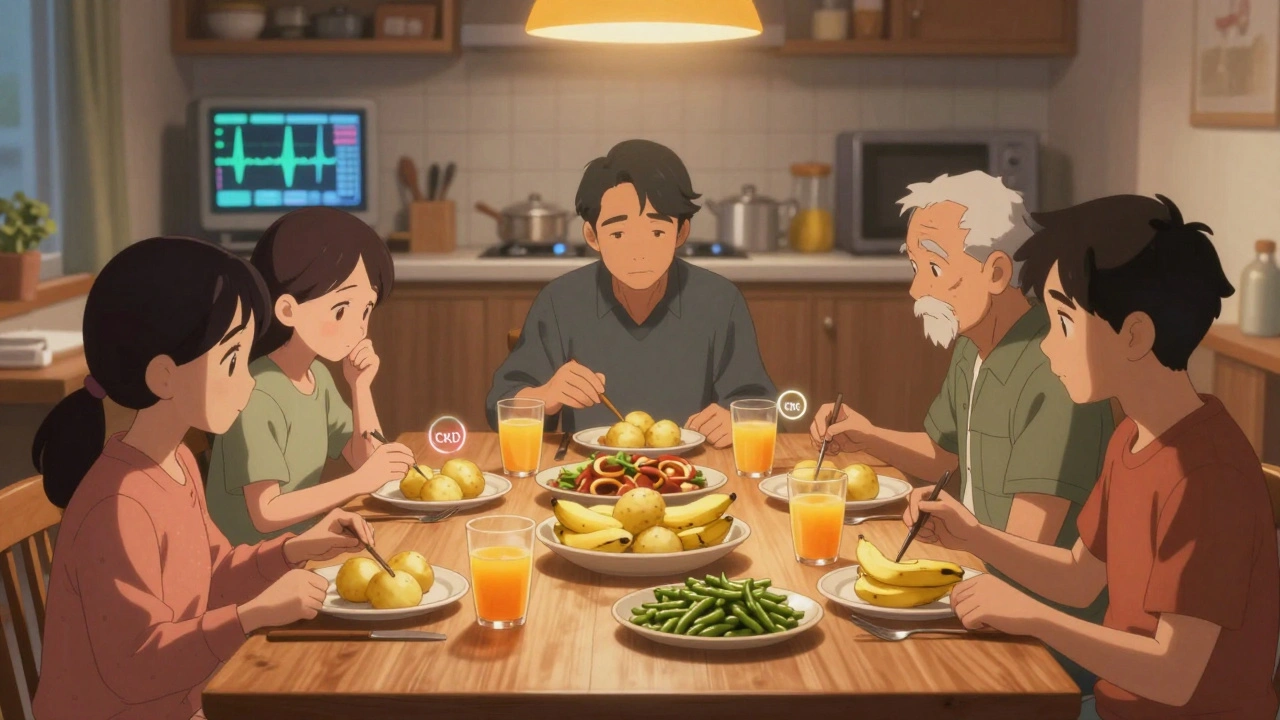
People with kidney disease, a condition where the kidneys lose their ability to filter waste and balance electrolytes. Also known as chronic kidney disease, it’s the most common cause of persistent hyperkalemia. When kidneys fail, they can’t excrete potassium the way they should. That’s why patients on dialysis are watched closely. But even early-stage kidney problems can lead to buildup if you eat too many potassium-rich foods—bananas, potatoes, spinach—or take supplements without knowing it. It’s not just about what you eat. It’s about what your body can handle.
Hyperkalemia doesn’t show up overnight. It creeps in slowly, often ignored because it doesn’t hurt. But the risk is real: irregular heartbeat, muscle paralysis, cardiac arrest. The good news? It’s preventable. Regular blood tests, knowing your meds, and adjusting your diet can keep you safe. You don’t need to avoid all potassium. You just need to know your limits.
Below, you’ll find real, practical posts that explain how medications like diuretics, ACE inhibitors, and spironolactone affect potassium levels—and what to do when things go wrong. You’ll also learn how to spot the warning signs before it’s too late, and how to talk to your doctor about testing and treatment. This isn’t theory. It’s what people actually face—and how they manage it.