When your kidneys aren’t working well, even simple foods can become dangerous. For people with chronic kidney disease (CKD), high potassium levels - a condition called hyperkalemia - can turn a quiet afternoon into a medical emergency. It’s not just about avoiding bananas. It’s about understanding what happens when your body can’t flush out potassium, how to react fast when levels spike, and how to live well without giving up everything you love to eat.
Why Hyperkalemia Is a Silent Threat in CKD
In healthy people, kidneys keep potassium balanced. But in CKD, especially stages 3b through 5, that system breaks down. Potassium builds up slowly, often without symptoms - until it doesn’t. By the time you feel muscle weakness, heart palpitations, or odd tingling, your potassium may already be above 5.5 mmol/L. At 6.0 mmol/L or higher, your heart rhythm can go haywire. ECG changes like peaked T-waves or a widened QRS complex are warning signs you can’t ignore. About half of people with advanced CKD not on dialysis will develop hyperkalemia at some point. The problem isn’t just the kidneys. It’s the medications. Drugs like ACE inhibitors, ARBs, and mineralocorticoid receptor antagonists (MRAs) protect your heart and kidneys - but they also raise potassium. Stopping them feels safer, but studies show it increases your risk of heart attack and kidney failure by up to 34%. You can’t afford to quit these drugs. You need better tools to manage the side effect.Dietary Limits: What You Can and Can’t Eat
There’s no one-size-fits-all diet for hyperkalemia. It depends on your kidney function. If you’re in early CKD (stages 1-3a), you don’t need to panic about every orange or potato. A “prudent but not restrictive” approach works best - meaning avoid extreme limits unless your doctor says otherwise. But if you’re in stage 3b or beyond, you’re looking at 2,000 to 3,000 mg of potassium per day. That’s less than half what most healthy adults eat. Here’s what that looks like in real food:- One medium banana = 422 mg
- One cup of orange juice = 496 mg
- One medium baked potato = 926 mg
- One cup of cooked spinach = 839 mg
- One cup of white rice = 50 mg
- One egg = 63 mg
Emergency Treatment: What Happens When Potassium Spikes
If your potassium hits 5.5 mmol/L or higher - especially with ECG changes - you need immediate action. This isn’t something to wait on. Emergency protocols are clear:- Calcium gluconate - 10 mL of 10% solution given slowly through an IV. This doesn’t lower potassium, but it protects your heart muscle from the electrical chaos. Onset: 1-3 minutes. Lasts 30-60 minutes.
- Insulin and glucose - 10 units of regular insulin with 50 mL of 50% dextrose. This pulls potassium into your cells. Works in 15-30 minutes. Lowers levels by 0.5-1.5 mmol/L. But watch for low blood sugar - it happens in 10-15% of cases.
- Sodium bicarbonate - if you’re also acidotic (bicarbonate <22 mmol/L), this helps shift potassium into cells. Works in 5-10 minutes.

Chronic Management: The New Generation of Potassium Binders
For long-term control, older treatments like sodium polystyrene sulfonate (SPS) are fading. SPS takes hours to work, causes constipation, and has a rare but deadly side effect: colonic necrosis. It also adds sodium - 11 mmol per gram - which can worsen swelling and high blood pressure. Two newer drugs have changed the game:- Sodium zirconium cyclosilicate (SZC, brand name Lokelma) - starts working in under an hour. Lowers potassium by 1.0-1.4 mmol/L in the first hour. Great for acute spikes. But it adds sodium - about 1.2 grams per day - which can cause fluid retention in heart failure patients (12.3% vs. 4.7% with patiromer).
- Patiromer (brand name Veltassa) - takes 4-8 hours to work. Less immediate, but better for daily use. It’s sodium-neutral, so it’s safer for people with heart failure or high blood pressure. Side effects? Constipation (14.2%) and low magnesium (18.7%). It’s also chalky and hard to swallow - 22% of patients quit because of taste and texture.
Monitoring, Timing, and Avoiding Mistakes
You can’t manage what you don’t measure. After starting or changing a RAASi drug, get your potassium checked within 1-2 weeks. Then every 3-6 months if stable. But if you feel weak, dizzy, or your heart skips - test right away. Timing matters with binders. Patiromer binds to other drugs. If you take levothyroxine for thyroid issues, take it at least 3 hours before or after patiromer. Same with antibiotics or diuretics. A pharmacist should review all your meds - people with CKD take an average of 7.2 medications. One wrong interaction can undo months of progress. Electronic alerts in medical records now trigger automatic referrals to dietitians and pharmacists when potassium hits 5.0 mmol/L or higher. Clinics using this system saw RAASi continuation rates jump from 52% to 81%.
What’s Next: Precision and Innovation
The future of hyperkalemia care is personal. Researchers are testing urine potassium tests to tailor diets exactly to your body’s needs - not just your kidney stage. New drugs like tenapanor, originally for phosphate control, are showing promise in lowering potassium with minimal side effects. By 2027, experts predict 75% of CKD patients on heart-protecting drugs will also be on a potassium binder. The cost is still a barrier - patiromer runs about $635 a month in the U.S., while SPS is under $50. But when you factor in the $12,450 average cost of a hyperkalemia hospitalization, the binders pay for themselves in under two years. Digital tools are helping too. Apps that scan groceries and track potassium intake are making diet management less overwhelming. One study found patients using them stuck to their plan 32% better than those relying on memory or paper lists.Bottom Line: Balance, Not Fear
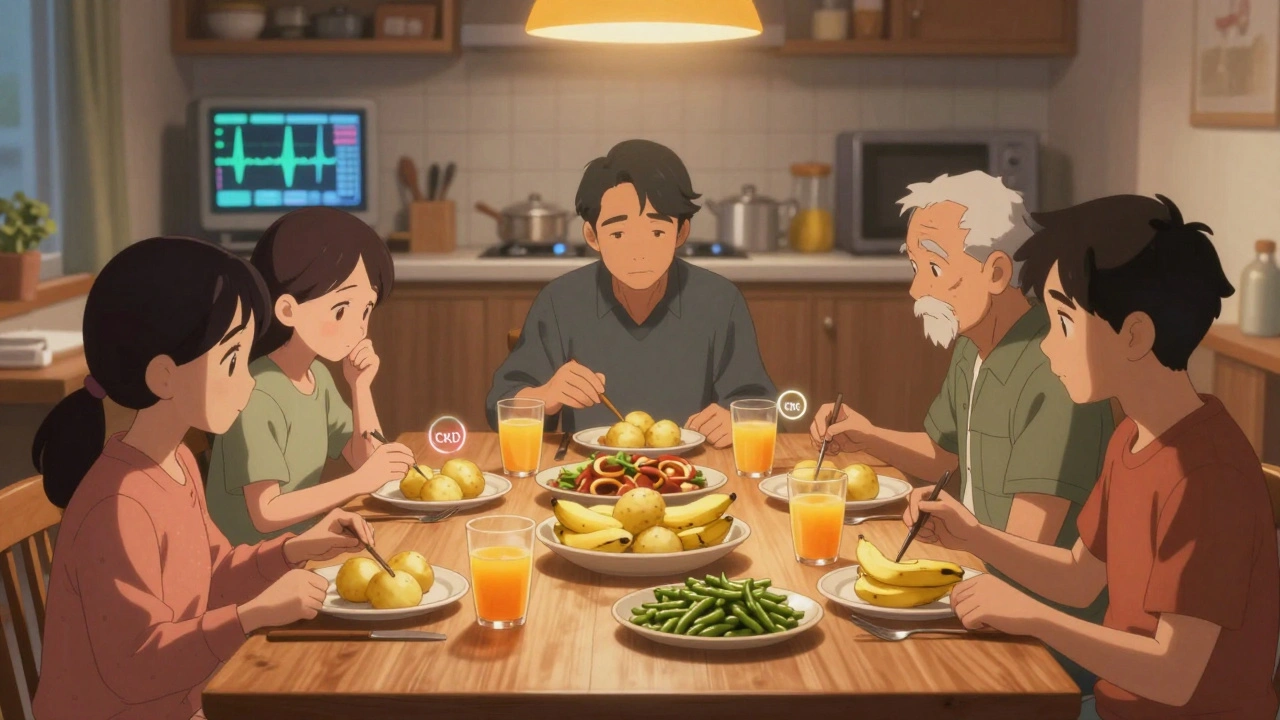
Hyperkalemia in CKD isn’t a death sentence. It’s a challenge - one that’s increasingly solvable. You don’t need to live on plain rice and boiled chicken forever. You need a plan: regular monitoring, smart food choices, and the right medications. New binders let you keep your life-saving drugs without risking your heart. Diet changes don’t have to be perfect - just consistent. And emergency treatment is fast, effective, and available when you need it. The goal isn’t to eliminate potassium. It’s to control it - so your kidneys don’t fail, your heart doesn’t race, and you can still enjoy a meal with your family.What is a safe potassium level for someone with CKD?
For most people with chronic kidney disease, a serum potassium level between 4.0 and 4.5 mmol/L is considered optimal. Levels above 5.0 mmol/L are considered elevated, and above 5.5 mmol/L require immediate medical attention. The goal isn’t to push potassium to the lowest possible number - it’s to stay in a range that protects your heart while allowing you to keep essential medications like ACE inhibitors or MRAs.
Can I still eat fruits and vegetables with CKD and hyperkalemia?
Yes, but you need to choose wisely and prepare them correctly. Low-potassium options include apples, grapes, cabbage, and green beans. Boiling vegetables like potatoes, carrots, or spinach cuts potassium by up to half. Drain and rinse canned foods. Avoid high-potassium fruits like bananas, oranges, and kiwis, or limit them to small portions. A renal dietitian can help you build a balanced plate that fits your needs.
Do potassium binders really work, and are they safe long-term?
Yes, newer binders like patiromer and sodium zirconium cyclosilicate are effective and safe for long-term use. Studies show they lower potassium reliably and help patients stay on life-saving heart and kidney medications. Long-term safety beyond 12-24 months is still being studied, but current data shows no major risks like organ damage. Side effects like constipation or sodium retention are manageable with monitoring and dose adjustments.
Why can’t I just stop my blood pressure meds if my potassium is high?
Stopping RAAS inhibitors (like lisinopril or losartan) might lower potassium, but it increases your risk of heart attack, stroke, and kidney failure by up to 34%. These drugs protect your heart and slow kidney damage - even more than they raise potassium. The solution isn’t quitting them - it’s using potassium binders and diet to safely keep them in your regimen. Most patients can stay on full doses with proper management.
How often should I get my potassium checked if I have CKD?
Check your potassium within 1-2 weeks after starting or changing any RAAS inhibitor, diuretic, or potassium binder. Once stable, testing every 3-6 months is usually enough. But if you feel weak, have palpitations, or get sick (like with vomiting or diarrhea), test immediately. Don’t wait for your next appointment - high potassium can strike fast.
Are there any natural ways to lower potassium besides diet?
No reliable natural methods exist. Diuretics like furosemide help only if your kidney function is still decent (eGFR above 30). Exercise can shift potassium into muscles temporarily, but it’s not a solution. Herbal supplements, salt substitutes, or “detox” teas often contain hidden potassium or can worsen kidney function. Stick to proven medical approaches: diet, binders, and monitoring - not unregulated remedies.
Jennifer Blandford
December 10, 2025 AT 15:34Just wanted to say this post saved my life. My dad’s in stage 4 CKD and we were terrified of every meal. Now we boil his veggies, use apps to track potassium, and actually eat dinner with the family again. Thank you.
Ronald Ezamaru
December 12, 2025 AT 07:42People don’t realize how dangerous stopping ACE inhibitors is. I’ve seen patients flatline because they thought ‘natural’ meant better. These meds aren’t optional - they’re life support for the heart. The potassium issue? Manage it. Don’t abandon the treatment.
Shubham Mathur
December 13, 2025 AT 15:44Boiling reduces potassium by half? That’s the trick I’ve been missing. I was avoiding spinach like it was poison. Now I boil it for 10 mins drain it rinse it and boom - I’m not a potato anymore. Also stop using salt substitutes they’re just potassium bombs in disguise. And no more coconut water unless you wanna visit the ER.
Rich Paul
December 15, 2025 AT 04:52So you’re telling me that if I’m on an SGLT2 inhibitor and an MRA and I eat a baked sweet potato I’m basically playing Russian roulette with my ventricles? Cool cool. And yet somehow my nephrologist still says ‘just eat normally’ like I’m a toddler with a juice box. This is why medicine is broken.
Iris Carmen
December 16, 2025 AT 15:41i was just gonna eat a banana and then i remembered oh right i have kidneys that are basically broken toaster ovens. now i eat rice and eggs like its a cult. also why does no one talk about how sad it is to watch your grandma cry because she cant have her mango smoothie anymore??
Ruth Witte
December 18, 2025 AT 03:47YOU CAN DO THIS 💪 One boiled potato at a time! You’re not giving up food - you’re upgrading your survival mode. And guess what? Your heart will thank you. I’ve been there. You got this. ❤️
Ryan Brady
December 19, 2025 AT 12:51My uncle died from this. They told him to cut back on bananas. He ate 5 a day. He thought he was ‘healthy’. America is dying from fake wellness culture. Stop pretending you’re a vegan warrior when your kidneys are failing. This post is 100% correct.
Raja Herbal
December 21, 2025 AT 01:14Oh so now we’re blaming potassium instead of the fact that our healthcare system doesn’t give a damn about chronic disease unless you’re in a hospital bed screaming? Funny how the same doctors who prescribe the drugs that cause this also tell you to ‘eat healthy’ like you’re on a cooking show.
Asset Finance Komrade
December 22, 2025 AT 08:38It is not merely a biochemical imbalance - it is a metaphysical confrontation with mortality. The potassium in the banana is not food - it is the echo of systemic neglect. We are all dying slowly, and the ECG is merely the universe’s way of whispering: ‘You were never meant to outlive your organs.’
Noah Raines
December 23, 2025 AT 02:18My wife’s on dialysis now. We learned the hard way. Boiling potatoes? Yes. Rinsing beans? Absolutely. But the real game-changer? Getting a dietitian on your team. Not just any one - someone who actually gets it. We found one through a CKD Facebook group. It changed everything. Don’t go it alone.
Delaine Kiara
December 23, 2025 AT 11:47Let me tell you something - the real tragedy isn’t hyperkalemia. It’s that we’ve turned nutrition into a military operation. You can’t just have a salad anymore? You need a spreadsheet? A barcode scanner? A blood test every Tuesday? What happened to eating food? This isn’t medicine - it’s performance art for anxious people who think they’re controlling their fate by counting milligrams.
Brianna Black
December 23, 2025 AT 18:05I’m a transplant recipient now - and I can’t tell you how much I miss the freedom of eating a peach without panic. But I also know this: the people who survive this? They’re not the ones who followed every rule perfectly. They’re the ones who found joy in small things - a spoonful of rice pudding, a cup of weak tea, a hug from someone who doesn’t judge. Don’t lose your humanity trying to save your kidneys.
Sarah Gray
December 25, 2025 AT 13:08There is a fundamental flaw in your presentation: you cite a 2023 survey without providing the source, sample size, or methodology. Furthermore, you imply that boiling vegetables reduces potassium by 50% - this is an oversimplification that varies by vegetable type, cut size, water volume, and boiling duration. This is irresponsible medical communication. I would not trust this advice in a clinical setting.
Stacy Tolbert
December 26, 2025 AT 21:31Thank you for writing this. I cried reading it. My mom’s been in CKD for 12 years. We’ve lost so many dinners. So many birthdays. So many family holidays. But we still eat. We still laugh. And sometimes, we just sit together in silence, holding hands, knowing she’s fighting. This post didn’t just give me facts - it gave me peace.