Potassium Safety Calculator
Assess Your Potassium Risk
This tool helps you calculate your total daily potassium intake and determine your risk level for hyperkalemia when using potassium-based salt substitutes with blood pressure medications.
Most people think swapping regular salt for a "heart-healthy" salt substitute is a smart move-especially if they’re on blood pressure medication. But if you’re taking an ACE inhibitor or an ARB, that simple swap could be putting your heart at serious risk. It’s not a myth. It’s not a warning you’ll see on the label. And most patients have no idea it’s happening.
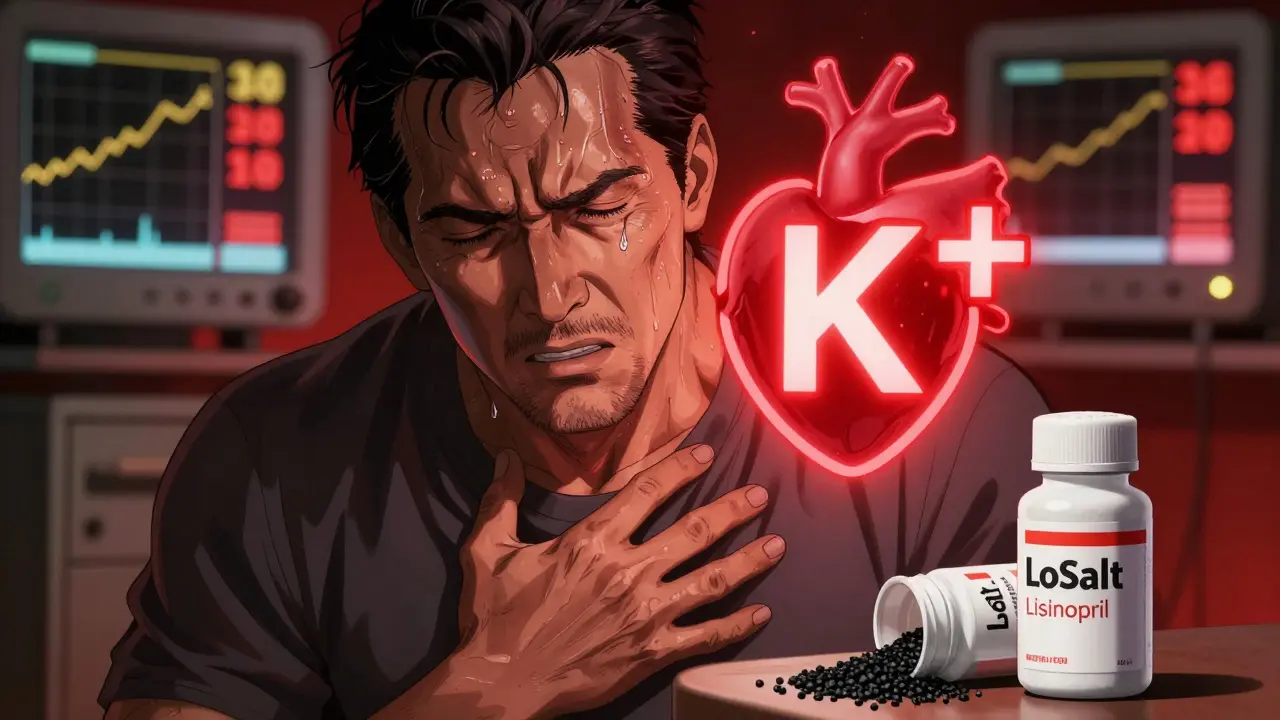
Here’s what’s really going on: Salt substitutes like LoSalt, NoSalt, or Heart Salt replace part or all of the sodium chloride in table salt with potassium chloride. On paper, it makes sense. Less sodium means lower blood pressure. More potassium means better heart rhythm and muscle function. But when your body can’t flush out the extra potassium-because you’re on an ACE inhibitor or ARB-the numbers start climbing. And when serum potassium hits 6.5 mmol/L or higher, your heart can stop beating. That’s not theoretical. It’s been documented in ER reports, case studies, and patient testimonials.
How ACE Inhibitors and ARBs Trap Potassium
ACE inhibitors and ARBs work by blocking parts of your body’s renin-angiotensin-aldosterone system. That’s a mouthful, but here’s the simple version: this system tells your kidneys to get rid of potassium. When it’s blocked, potassium sticks around. That’s actually helpful for people with heart failure or kidney damage-it reduces strain on the heart. But when you add a potassium-rich salt substitute on top of that, your body gets overwhelmed.
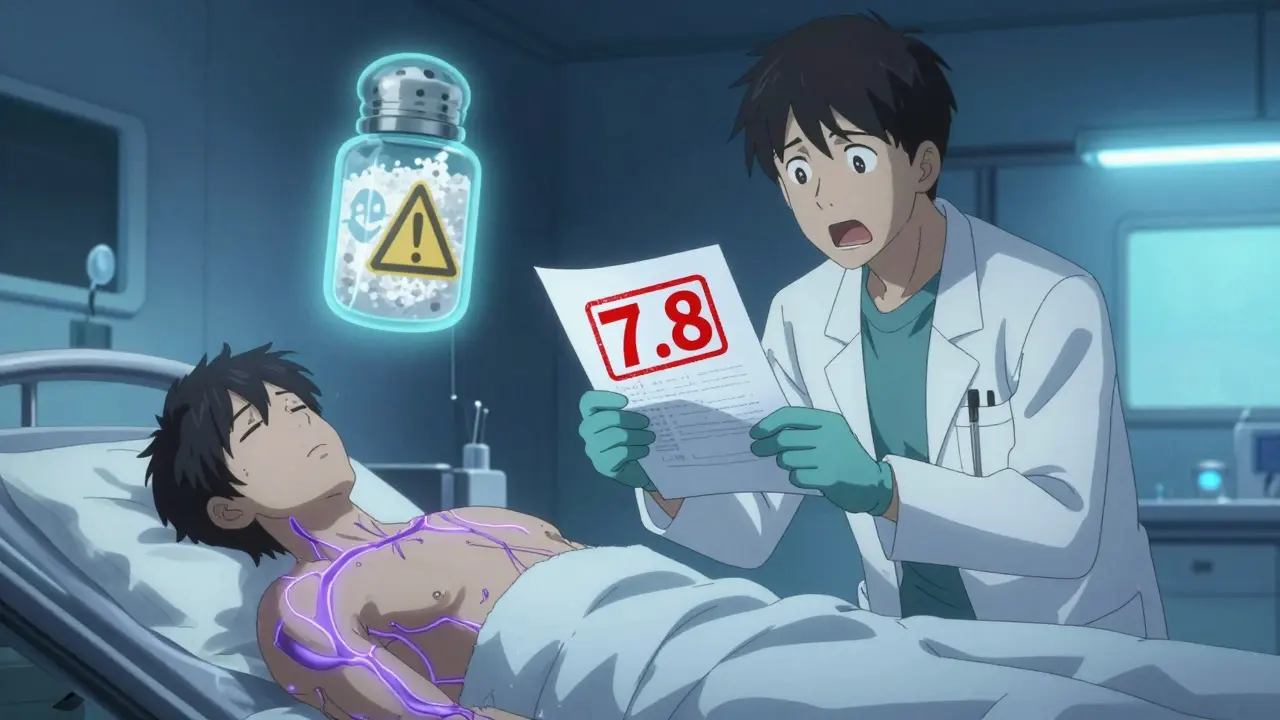
Think of it like a clogged drain. Your kidneys are the pipes. ACE inhibitors and ARBs slow down the flow. Potassium chloride from your salt substitute pours in like a flood. The result? Hyperkalemia. That’s when potassium levels in your blood rise dangerously high. Levels above 5.0 mmol/L are considered high. Above 6.5 mmol/L? That’s a medical emergency. One 2004 case report in the Journal of the Royal Society of Medicine described a 72-year-old man who suffered cardiac arrest after using LoSalt while taking lisinopril. His potassium level? 7.8 mmol/L.
Who’s at Risk? It’s More Common Than You Think
You might think this only affects older people with kidney disease. But the numbers say otherwise. In the U.S., about 15% of adults have chronic kidney disease (CKD), according to CDC 2022 data. That’s 37 million people. And nearly 40% of hypertension patients are prescribed an ACE inhibitor or ARB, per the American College of Cardiology. That means millions of people are already on these medications-and many are using salt substitutes without knowing the danger.
Even more alarming: 14.5% of U.S. adults have an estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73m², meaning their kidneys aren’t filtering well. That’s the sweet spot where potassium starts building up fast. And here’s the kicker: many of these people don’t even know they have reduced kidney function. It shows up on routine blood work, but unless your doctor checks for it, you’re flying blind.
Diabetic patients are another high-risk group. About 10-20% of diabetics with kidney disease have hyporeninemic hypoaldosteronism-a condition where the body doesn’t make enough aldosterone to push potassium out. The American Diabetes Association specifically warns this group faces “disproportionately high hyperkalemia risk” when combining salt substitutes with ACE inhibitors or ARBs.
The Numbers Don’t Lie: How Much Potassium Are You Really Getting?
Let’s get specific. One-quarter teaspoon of table salt gives you about 1,500 mg of sodium. If you replace half of that with a potassium chloride substitute like Lite Salt (50% sodium, 50% potassium), you’re cutting sodium by 315 mg-but adding 525 mg of potassium. That’s a net gain of over half a gram of potassium just from your seasoning.
Most people get about 2,800 mg of potassium daily from food-bananas, potatoes, spinach, beans, yogurt. That’s already near the recommended upper limit. Add 500 mg from your salt substitute, and you’re pushing close to 3,300 mg. For someone with healthy kidneys, that’s fine. For someone on an ACE inhibitor? That’s enough to tip the scale.
A 2019 analysis in Hypertension showed that potassium-enriched salt substitutes can raise daily potassium intake by 525 mg on average. That might sound small, but in someone with impaired kidney function, it’s enough to trigger dangerous spikes. One patient in a Reddit thread from October 2023 reported waking up in the ER with a potassium level of 6.3 after using “Heart Salt” for just three weeks while on lisinopril.

It’s Not Just About Salt: Other Hidden Sources
Most people think the danger is only in the salt shaker. But potassium chloride is also added to low-sodium processed foods, meal replacements, sports drinks, and even some “healthy” snack bars. If you’re eating packaged foods labeled “reduced sodium,” check the ingredients. You’ll often see “potassium chloride” right after “sodium chloride.”
And don’t assume “no salt added” means safe. That just means no sodium chloride. It doesn’t mean no potassium chloride. The label doesn’t have to say “contains potassium.” It’s not required. In fact, the FDA’s Dr. Lisa M. Wruck told Congress in September 2023 that only 3 out of 12 major salt substitute brands clearly warn against use with ACE inhibitors or ARBs.
What Does the Science Say? Benefits vs. Risks
There’s no denying that reducing sodium helps lower blood pressure. And potassium does have cardiovascular benefits. A landmark 2025 JAMA Network study followed 21,000 people and found that using salt substitutes with 25% potassium chloride reduced stroke recurrence by 14% over five years. That’s huge. But here’s what the study didn’t say: it excluded people with advanced kidney disease or those on ACE inhibitors/ARBs.
That’s the problem. The benefits apply to healthy people. The risks are concentrated in a smaller, high-risk group. The Chronic Kidney Disease Prognosis Consortium found that while hyperkalemia occurred in just 0.8 cases per 100 person-years in the general population using salt substitutes, it jumped to 8.7 cases per 100 person-years in CKD patients on ACE inhibitors. That’s more than ten times the risk.
Dr. Sarah Anderer, lead author of the JAMA study, says potassium substitutes are safe for most people. Dr. Mark S. Segal, a nephrologist, disagrees. He says those findings don’t apply to patients with advanced kidney disease. Both are right. The issue isn’t the salt substitute-it’s the combination.
What Should You Do? A Practical Guide
If you’re on an ACE inhibitor or ARB, here’s what you need to do right now:
- Check your salt substitute. Look at the ingredients. If it says “potassium chloride,” stop using it immediately.
- Ask your doctor for a recent potassium blood test. If your last test was more than 6 months ago, get one now. Normal is 3.5-5.0 mmol/L. Anything above 5.0 needs attention.
- Ask if your kidney function is normal. Request your eGFR number. If it’s below 60, avoid potassium chloride entirely.
- Switch to herb-based flavorings. Use Mrs. Dash, garlic powder, onion powder, smoked paprika, lemon zest, or fresh herbs. These reduce sodium by 15-20% with zero potassium risk.
- Don’t assume “natural” means safe. Some sea salts, Himalayan salts, or “mineral salts” are marketed as healthier. But they still contain sodium. And if they’re labeled “low sodium,” they may contain potassium chloride-hidden in plain sight.
The National Kidney Foundation’s 2023 guidelines say doctors should screen every patient on ACE inhibitors or ARBs for salt substitute use during every visit. But a 2023 JAMA Internal Medicine study found 78% of patients on these meds had no idea dietary potassium could be dangerous. That’s a system failure. Don’t wait for your doctor to ask. Ask yourself.
What Are the Alternatives?
You don’t have to give up flavor. You just have to change your approach.
- Herbs and spices: Cumin, coriander, oregano, rosemary, thyme, turmeric, ginger, chili flakes. These add depth without potassium.
- Acidic ingredients: Lemon juice, lime juice, vinegar (balsamic, apple cider, rice wine). They brighten flavor and reduce the need for salt.
- Umami boosters: Mushroom powder, tomato paste, soy sauce (low-sodium version), nutritional yeast. They give savory depth without sodium or potassium overload.
- Low-sodium broths: Use homemade or certified low-sodium versions for soups and stews.
One 2023 survey of 1,247 users on HealthyLowSodium.com found that 87% improved their blood pressure using herbs and spices-without ever touching a potassium salt substitute. And none reported hyperkalemia.
What’s Changing? The Future of Salt Substitutes
Change is coming-but slowly. In Canada, food regulators now require salt substitutes to carry a clear warning: “Contraindicated in patients taking ACE inhibitors.” That rule started January 1, 2024. The U.S. FDA announced proposed rulemaking in May 2024 to require similar labeling. Final rules are expected in Q2 2026.
Meanwhile, companies are experimenting with new formulations. NutraTech Solutions is testing a slow-release potassium formulation in the K-SAFE trial, which could deliver potassium benefits without the dangerous spikes. Results won’t be out until late 2026.
For now, the safest bet is simple: if you’re on an ACE inhibitor or ARB, don’t use potassium-based salt substitutes. Period. There are safer, equally effective ways to reduce sodium. You don’t need to risk your life for a flavor shortcut.
When to Seek Immediate Help
Hyperkalemia doesn’t always cause symptoms. But when it does, they’re subtle-and easily mistaken for fatigue or aging. If you’re on an ACE inhibitor or ARB and you start experiencing:
- Unexplained muscle weakness or cramps
- Irregular heartbeat or palpitations
- Nausea or dizziness
- Feeling unusually tired or faint
Get your potassium checked immediately. Don’t wait. Don’t assume it’s “just stress.” Call your doctor or go to urgent care. A simple blood test can save your life.
Jake Moore
January 17, 2026 AT 15:51Just had my potassium checked last month-5.2. Was using Lite Salt for months thinking I was being healthy. My cardiologist nearly had a heart attack. This post saved my life. Stop using those substitutes if you're on an ACE inhibitor. Period.
Eric Gebeke
January 19, 2026 AT 00:48Wow. Another one of those ‘well-meaning’ health trends that’s just a slow-motion suicide pact. People don’t read labels. They don’t ask questions. They just buy what’s stamped ‘heart-healthy’ like it’s some kind of holy grail. You think your grandma’s ‘natural’ salt substitute is safe? It’s not. It’s just a potassium time bomb with a nice label. And now you’re mad at the system? No, you’re mad because you didn’t do your own damn research.
Joni O
January 20, 2026 AT 14:35I’m so glad I found this. I’ve been on lisinopril for 5 years and switched to NoSalt last year because my doc said ‘cut sodium.’ Never once did they mention potassium. I just checked my last bloodwork-5.4. I’m canceling my Amazon order for that stuff today. Thanks for the wake-up call. I’ll start using garlic powder and lemon zest instead. 🙏
Ryan Otto
January 21, 2026 AT 08:14This is a textbook case of institutional negligence. The FDA has known about this for decades. The pharmaceutical industry profits from both the drugs and the complications they cause. Salt substitutes? A distraction. A manufactured crisis to keep you buying more meds. The real danger isn’t potassium-it’s the system that lets this go unregulated. And don’t get me started on how they quietly removed potassium warnings from packaging after lobbying. This isn’t an accident. It’s corporate malfeasance dressed up as ‘health advice.’
Andrew Qu
January 22, 2026 AT 21:29Good breakdown. One thing to add: even if your eGFR is above 60, if you’re diabetic or over 65, your kidneys may be less efficient than the numbers suggest. I’ve seen patients with ‘normal’ labs crash into hyperkalemia after switching to potassium salt. Bottom line: if you’re on an ACE/ARB, assume you’re at risk until proven otherwise. Get tested. Don’t guess. And ditch the salt substitute-your heart will thank you.
kenneth pillet
January 23, 2026 AT 10:59Just checked my pantry. Had a bag of ‘Lite Salt.’ Tossed it. Going back to regular salt and using herbs. My BP’s been stable anyway. Maybe the salt wasn’t the problem. My stress was.
Jay Clarke
January 25, 2026 AT 07:37Let’s be real-this isn’t about salt. This is about control. The medical industrial complex wants you to believe you’re powerless. That you can’t flavor your food without a prescription. That you’re too stupid to know what’s safe. But you’re not. You’re a human being with taste buds and a brain. Stop letting them sell you fear wrapped in a label. Use sea salt. Use vinegar. Use love. Your body knows what to do if you stop poisoning it with corporate ‘solutions.’
Selina Warren
January 26, 2026 AT 21:29They told me to ‘eat more potassium’ for years. Bananas, spinach, sweet potatoes. Then they gave me lisinopril and told me to stop using salt. No one connected the dots. I thought I was doing everything right. Then I started getting dizzy after meals. Turns out my potassium was 6.1. I almost died because I trusted the system. Now I cook with smoked paprika and lemon. And I scream at every doctor who says ‘just cut salt.’ You need to think. You need to ask. You need to read the damn label. Don’t be like me.
Nishant Sonuley
January 28, 2026 AT 21:02As someone from India where ‘rock salt’ and ‘black salt’ are staples, I’ve seen this play out for decades. Grandmas use kala namak thinking it’s ‘natural’-but it’s still sodium chloride with trace minerals. The real villain is the silent potassium chloride in those ‘low sodium’ packaged snacks and protein bars. I’ve had patients on ARBs who eat ‘healthy’ meal replacements daily and end up in ICU. The problem isn’t the salt shaker-it’s the entire food industry’s deception. We need better labeling. We need education. And we need doctors to stop assuming patients know what’s in their food. Most don’t. And that’s not their fault.
Emma #########
January 29, 2026 AT 17:38I’m so relieved I found this. My mom’s on losartan and uses LoSalt every day. I’ve been trying to tell her for months. She said, ‘But it’s better for my heart!’ I printed this out and gave it to her. She cried. Then she threw the salt away. Thank you for writing this. It’s not just information-it’s a lifeline.
Andrew McLarren
January 29, 2026 AT 21:11While the clinical evidence presented is compelling and the risks are well-documented, it is also imperative to acknowledge the broader public health implications of sodium reduction. The population-level benefit of salt substitutes in reducing cardiovascular mortality is substantial, and the risk stratification must be carefully implemented to avoid overgeneralization. A blanket prohibition may inadvertently discourage beneficial dietary modifications among the majority of users who are not at risk. Precision medicine, not one-size-fits-all warnings, is the ethical imperative here.
Andrew Short
January 30, 2026 AT 09:53Of course they didn’t warn you. The FDA doesn’t care about you. They care about lawsuits and pharmaceutical profits. You think they’d put a warning on a product that could kill people? No. They’d rather you die quietly so they can keep selling you the next ‘miracle’ drug. This is why I don’t trust any government health advice. They’re all in bed with Big Pharma. You want to be safe? Don’t take their drugs. Don’t use their ‘healthy’ products. Just eat real food. Meat. Veggies. Water. That’s it. Everything else is poison with a label.
christian Espinola
January 31, 2026 AT 01:24There’s a 2023 meta-analysis in The Lancet that shows potassium chloride substitutes reduce all-cause mortality by 11% in normotensive populations. You’re cherry-picking high-risk cases to scare people. The real danger is fear-mongering. Don’t panic. Get tested. If your potassium is normal, you’re fine. If not, stop the substitute. But don’t throw out a proven public health tool because of a small subset of vulnerable patients. That’s not science. That’s hysteria.