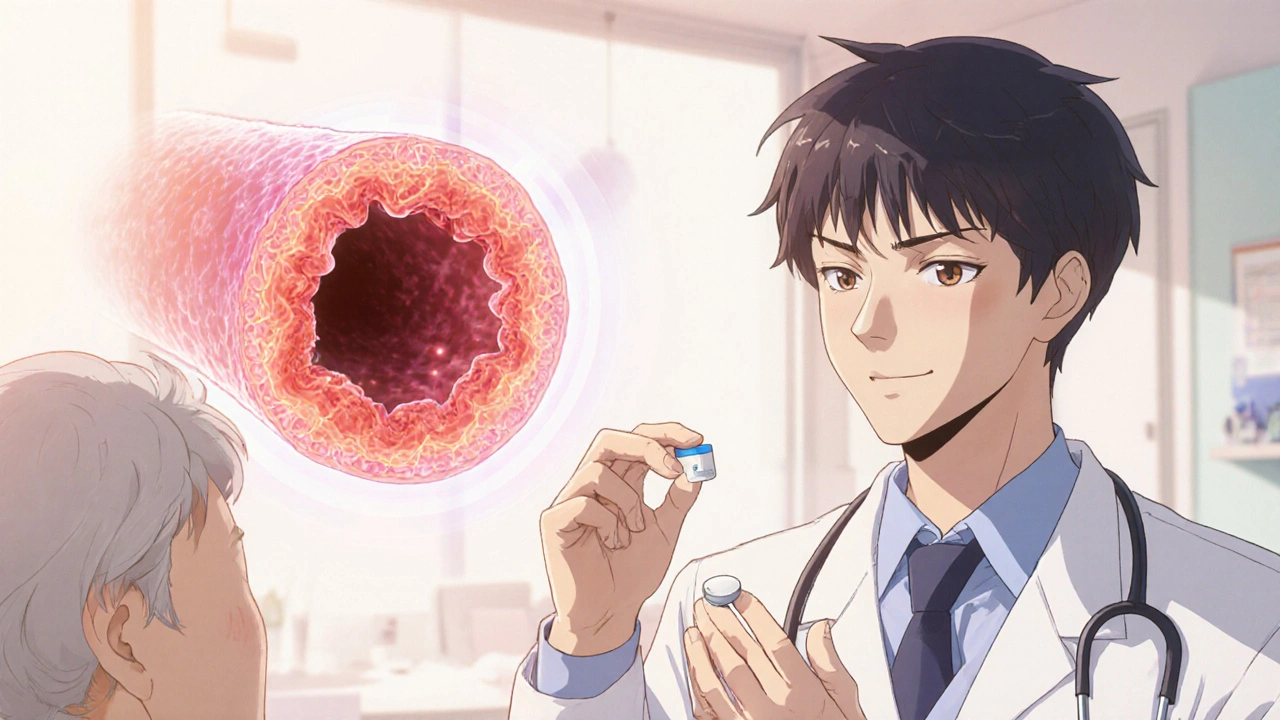
Aspirin and Vasculitis: Can It Help Reduce Inflammation and Pain?
Explore how aspirin may aid inflammation and pain in vasculitis, covering mechanisms, evidence, dosing, risks, and practical tips for safe use.
Read MoreWhen your vasculitis, a group of disorders causing inflammation in blood vessels. Also known as inflammatory vasculopathy, it can narrow or block arteries and veins, cutting off blood flow to vital organs. This isn’t just a vague ache—it’s a serious condition that can lead to organ damage if left unchecked. Vasculitis isn’t one disease; it’s a family of over 20 types, each targeting different vessel sizes and body areas. Some affect only the skin, others hit the kidneys, lungs, or nerves.
It often starts as an autoimmune disease, when the immune system mistakenly attacks healthy tissue. Your body turns on itself, sending immune cells to attack the walls of your blood vessels. Why? In many cases, no one knows for sure. But infections, certain medications, or even cancers can trigger it. People with rheumatoid arthritis or lupus are more likely to develop it too—because their immune systems are already on edge.
The symptoms? They’re all over the map. Fever, fatigue, weight loss—these are the quiet signs. Then come the red flags: purple spots on legs, numbness in fingers, chest pain, or sudden vision loss. If you’re losing feeling in your feet or have unexplained headaches after 50, it’s worth asking about vasculitis. Doctors look for patterns: which vessels are inflamed, which organs are involved, and how fast things are worsening. Blood tests, biopsies, and imaging like angiograms help pin it down.
Treatment starts with stopping the attack. corticosteroids, powerful anti-inflammatory drugs like prednisone. are the first line. They work fast but come with weight gain, bone loss, and mood swings. For longer-term control, doctors often add drugs like cyclophosphamide or rituximab—these calm the immune system without the steroid side effects. Newer biologics are changing the game, letting some people reduce or even stop steroids entirely.
What you won’t find in the posts below? Generic advice like "eat more greens" or "take supplements." These aren’t miracle cures. What you will find are real comparisons: how prednisolone stacks up against other steroids, how anticoagulants are used cautiously in vasculitis patients with clots, and why certain antibiotics or antivirals might be needed if an infection triggered the flare. You’ll see how people manage daily life with nerve damage, kidney issues, or skin ulcers—and what actually helps.
There’s no one-size-fits-all fix. Some forms fade away after a few months. Others need lifelong monitoring. But knowing what you’re dealing with—whether it’s giant cell arteritis, granulomatosis with polyangiitis, or something rarer—makes all the difference. The posts here aren’t theory. They’re practical, real-world breakdowns from people who’ve been there, and doctors who’ve treated them.
Below, you’ll find detailed comparisons of medications used to treat vasculitis and its complications—what works, what doesn’t, and what to watch out for. No fluff. Just what you need to understand your options and talk to your doctor with confidence.
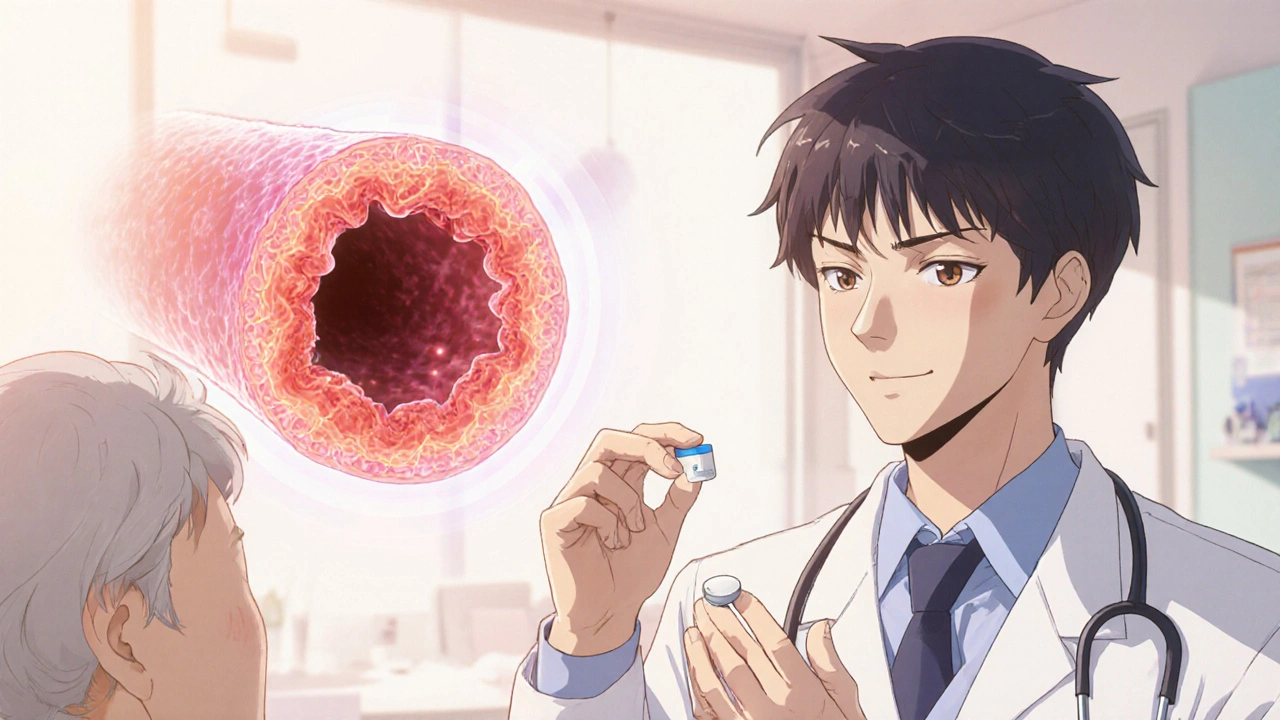
Explore how aspirin may aid inflammation and pain in vasculitis, covering mechanisms, evidence, dosing, risks, and practical tips for safe use.
Read More