Medication-Induced Aplastic Anemia: Causes, Risks, and What You Need to Know
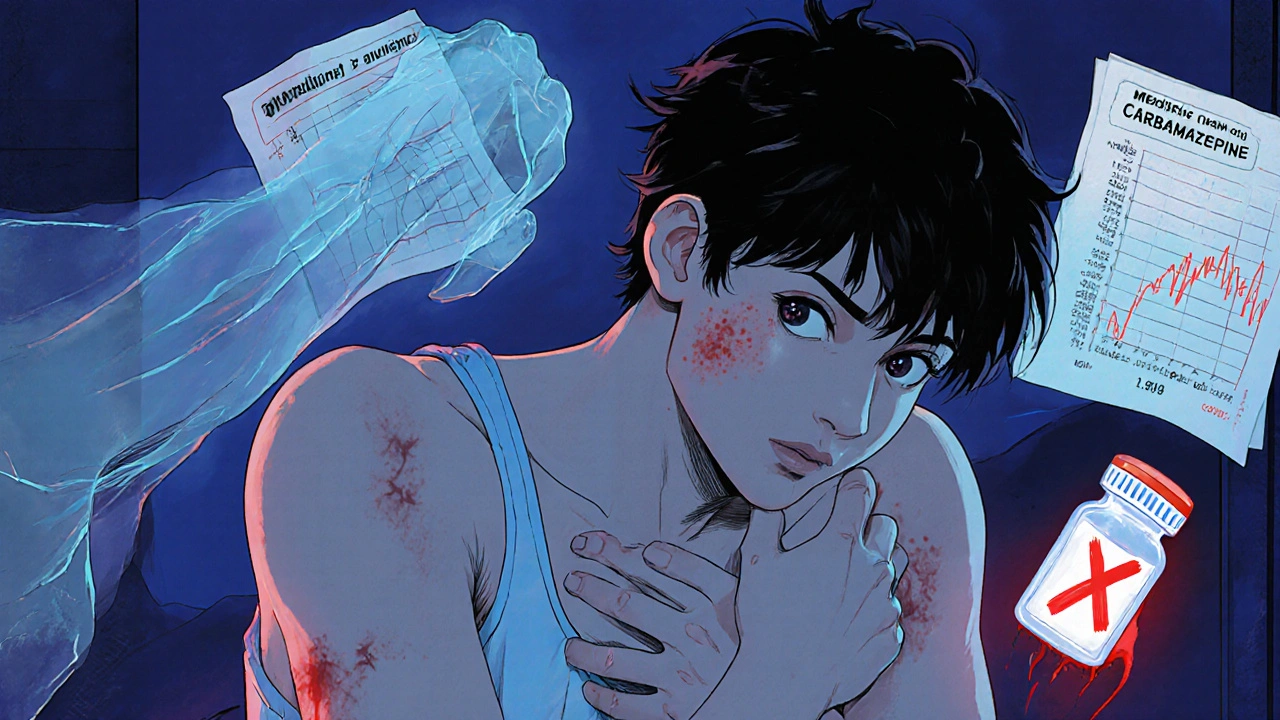
When a drug stops your bone marrow from making enough blood cells, it can trigger medication-induced aplastic anemia, a rare but life-threatening condition where the bone marrow fails to produce red blood cells, white blood cells, and platelets. Also known as drug-induced bone marrow failure, this isn’t just a side effect—it’s a systemic collapse that can leave you vulnerable to infection, bleeding, and extreme fatigue. Unlike inherited forms, this type happens because a medication directly damages the stem cells in your marrow. It doesn’t affect everyone, but when it does, the consequences are severe.
Some of the most common culprits include chemotherapy drugs, powerful agents used to kill cancer cells but also capable of wiping out healthy bone marrow, and immunosuppressants, medications that calm the immune system but sometimes turn it against the body’s own blood-producing cells. Antibiotics like chloramphenicol, anti-seizure drugs such as phenytoin, and even some NSAIDs have been linked to cases. It’s not about dosage alone—sometimes, it’s your unique biology reacting to a drug you’ve taken for months without issue. The timing is unpredictable: symptoms can appear weeks or even years after starting treatment.
Most people don’t realize their fatigue or bruising is tied to a drug they’re taking. A simple blood test showing low counts across the board—hemoglobin, white cells, platelets—is the first red flag. If your doctor suspects medication-induced aplastic anemia, they’ll likely order a bone marrow biopsy to confirm the diagnosis. Stopping the drug is the first step, but recovery isn’t guaranteed. Some patients bounce back on their own; others need transfusions, immune-suppressing therapy, or even a stem cell transplant.
What you’ll find in the posts below isn’t just a list of drugs that might cause this. It’s a practical guide to recognizing early signs, understanding which medications carry hidden risks, and learning how to protect yourself if you’re on long-term treatment. You’ll see real cases, how doctors track these reactions, and what alternatives exist when a drug turns dangerous. This isn’t theoretical—it’s about knowing what to watch for before it’s too late.