Most people don’t think about their medications doing more than treating an infection or calming a seizure. But some drugs can quietly shut down your bone marrow - the factory inside your bones that makes red blood cells, white blood cells, and platelets. When this happens, you don’t just feel tired. You’re at risk of life-threatening infections, uncontrolled bleeding, and organ failure. Medication-induced aplastic anemia is rare, but when it strikes, speed saves lives.
What Exactly Is Medication-Induced Aplastic Anemia?
Aplastic anemia isn’t just low blood counts. It’s when your bone marrow stops working - not because of cancer, not because of radiation, but because a drug damaged the stem cells that make new blood. The result? Pancytopenia: everything drops at once - hemoglobin, white cells, platelets. This isn’t a side effect you can shrug off. It’s a medical emergency.
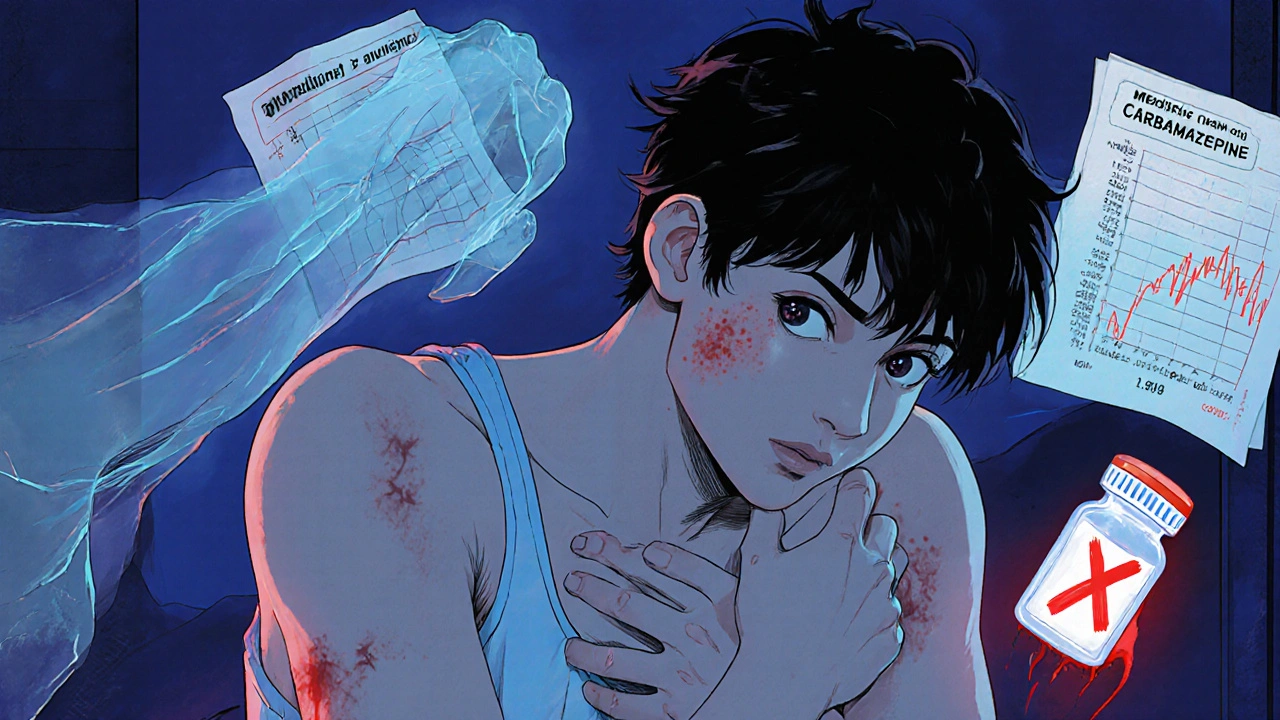
Some drugs cause this by directly poisoning bone marrow cells. Chloramphenicol, an old antibiotic, is the classic example. Back in the 1950s, doctors noticed patients on this drug were suddenly collapsing from infections and bleeding. Today, it’s rarely used, but the pattern holds: certain medications trigger immune attacks on stem cells. Carbamazepine, used for epilepsy and nerve pain, is one of the biggest modern culprits. It tricks your immune system into seeing your own marrow as a threat.
Other offenders include sulfonamide antibiotics, phenytoin, gold salts (used for arthritis), some NSAIDs like celecoxib, and even certain antipsychotics. Chemotherapy causes bone marrow suppression - that’s expected. But true aplastic anemia? That’s when the marrow doesn’t bounce back, even after stopping the drug. About 1-2% of chemo patients face this. It’s not common, but when it happens, it’s devastating.
Early Signs You Can’t Ignore
The worst part? The first signs are easy to miss. You think you’re just stressed, coming down with a bug, or getting older. But here’s what to watch for - especially if you’ve started a new medication in the last 4 to 8 weeks.
- Persistent fatigue that doesn’t improve with rest. Not just tired after work - exhausted by 10 a.m. after sleeping 8 hours.
- Unexplained bruising. Not from bumping into a door. Multiple bruises appearing for no reason, especially on your arms and legs.
- Recurrent low-grade fevers (99-101°F). No cough, no sore throat - just a fever that keeps coming back.
- Minor cuts that won’t stop bleeding. Or nosebleeds that last longer than 10 minutes.
- Unintentional weight loss - 5 to 10 pounds over 2-3 weeks without trying.
- Shortness of breath during simple tasks like walking to the mailbox.
These aren’t random symptoms. They’re your body screaming that your blood is failing. Studies show patients often wait 4-6 weeks before seeking help. By then, counts may have dropped 40-50%. The earlier you act, the better your odds.
What to Do Immediately If You Suspect It
There’s no time for waiting. If you’re on a high-risk drug and notice even two of these signs, take action now.
- Stop the medication. Do not wait for your doctor’s approval. Discontinuing the drug is the single most important step. In mild cases, blood counts can start climbing back within 4 weeks after stopping.
- Get a CBC test within 24 hours. This isn’t optional. A complete blood count will show if your hemoglobin, neutrophils, and platelets are dropping. Normal hemoglobin is 12-16 g/dL. Below 10? That’s a red flag. Neutrophils below 1,500/μL? Platelets below 150,000/μL? You need a hematologist now.
- Go to the ER if you have a fever above 100.4°F (38°C). This is a medical emergency. With low white cells, even a harmless cold can turn deadly. You’ll need antibiotics immediately and possibly isolation to avoid infection.
- Call a hematologist. Don’t wait for a referral. Find one yourself. Hospitals in major cities have specialized bone marrow failure clinics. If you’re in a rural area, ask your pharmacist - they’re often the first to spot the pattern.
Don’t assume your doctor will catch it. A 2022 Medscape survey found only 47% of family doctors could name the top five drugs linked to aplastic anemia. You have to be your own advocate.
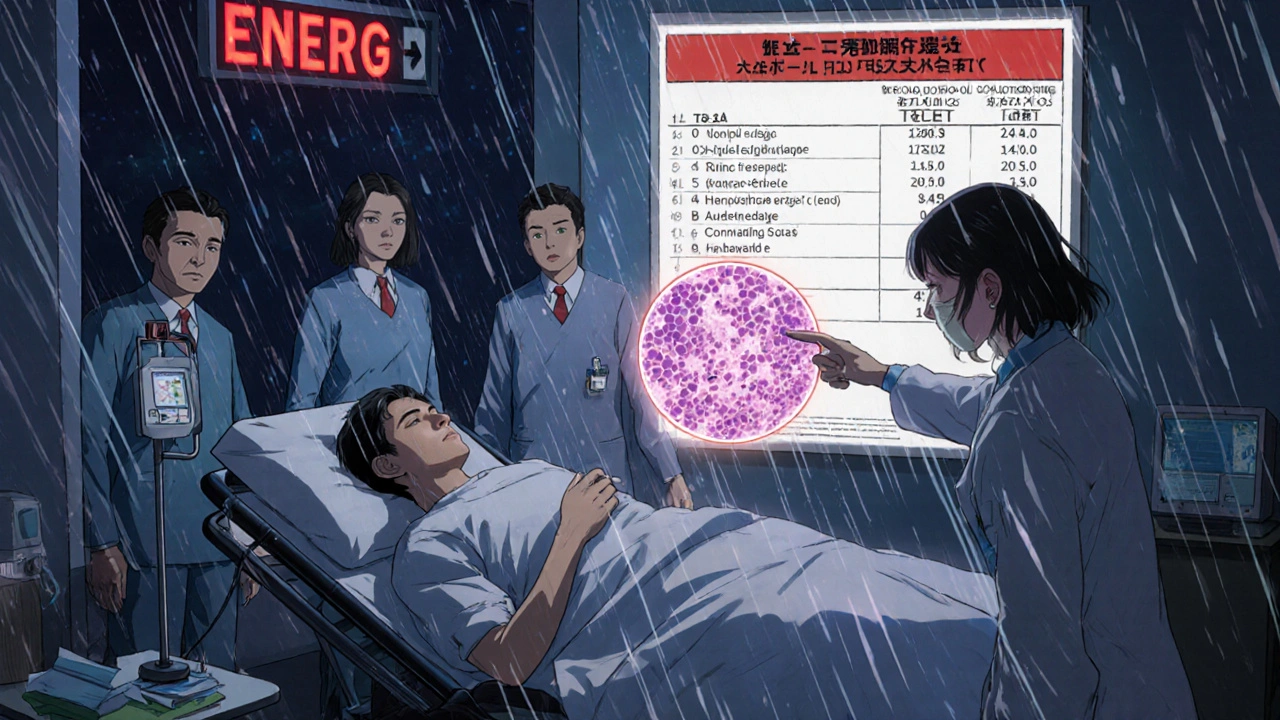
How Doctors Confirm the Diagnosis
A CBC is just the first step. If counts are low, they’ll order a bone marrow biopsy - the only way to know for sure. A normal marrow is packed with cells. In aplastic anemia, it’s mostly empty - less than 25% cellularity. That’s the gold standard.
They’ll also check your reticulocyte count - immature red blood cells. If it’s below 40,000/μL, your marrow isn’t trying to fix itself. That’s a sign of true failure, not just temporary suppression.
They’ll rule out other causes: vitamin B12 deficiency, liver disease, autoimmune disorders. But if you’re on a known risky drug, and your marrow is hypocellular, and your counts haven’t bounced back after stopping it - that’s medication-induced aplastic anemia.
What Happens After Diagnosis?
Treatment depends on severity. If your neutrophils are above 500/μL and platelets above 20,000/μL, stopping the drug and close monitoring might be enough. Many patients recover fully.
But if you’re in the severe range - neutrophils under 500, platelets under 20,000 - you need aggressive treatment. The standard is immunosuppressive therapy: horse anti-thymocyte globulin (ATG) plus cyclosporine. This calms your immune system so it stops attacking your marrow. In recent studies, this works in 78% of medication-induced cases.
If you’re young and have a matched sibling donor, a bone marrow transplant is the best long-term cure. It’s risky, but survival rates now exceed 85% when done early.
And here’s the critical warning: never restart the drug. Even if you recovered, restarting it has a 90% chance of triggering an even worse relapse. That’s not a risk worth taking.

Who’s at Risk - And How to Prevent It
You don’t need to avoid all medications. But if you’re starting one of these, ask your doctor about monitoring:
- Chloramphenicol (rare, but highest risk)
- Carbamazepine (for seizures, nerve pain)
- Phenytoin
- Sulfonamide antibiotics (like Bactrim)
- Gold compounds (for rheumatoid arthritis)
- Certain NSAIDs (long-term use)
- Some antipsychotics
For high-risk patients, the Mayo Clinic recommends a baseline CBC before starting, then weekly blood tests for the first 4 weeks. That’s not standard everywhere - but you can ask for it. If your clinic can’t do same-day CBCs, go to a lab that can.
Keep a written list of every medication you take - including doses and start dates. Patients who did this reduced diagnostic delays by over 6 days on average. Use a phone app - the AAMDS Foundation has one that tracks symptoms and blood counts. Users saw a 40% drop in delays.
And if you’re on chemotherapy, know that true aplastic anemia is rare. But if your counts don’t recover after treatment ends, push for a bone marrow biopsy.
Why This Matters More Than You Think
Medication-induced aplastic anemia is preventable. But it’s underdiagnosed. Only 28% of cases are caught at first visit. Most patients are told they have the flu, stress, or anemia from iron deficiency. By the time they get to a specialist, it’s too late for simple fixes.
The cost is high - over $50,000 for mild cases, half a million for transplants. But the human cost is higher. Dr. Neal Young from the NIH says survival drops from under 10% to 45% when diagnosis is delayed beyond 8 weeks. That’s not just a statistic. That’s someone’s parent, sibling, child.
Knowledge is your shield. If you’re on a risky drug, learn the signs. Don’t wait for someone else to notice. If your body feels wrong, get tested. Your life might depend on it.
Can over-the-counter drugs cause aplastic anemia?
Yes. While most cases come from prescription drugs like carbamazepine or chloramphenicol, long-term use of certain NSAIDs - such as celecoxib or phenylbutazone - has been linked to aplastic anemia. Even though they’re available without a prescription, they can still damage bone marrow in rare cases, especially with prolonged use or in genetically susceptible individuals.
How long after stopping the drug does recovery take?
Recovery time varies. In mild cases, blood counts may start improving within 2-4 weeks after stopping the medication. Full recovery can take 3-6 months. In severe cases, recovery depends on treatment like immunosuppressive therapy or transplant. Some patients never fully recover without intervention.
Is aplastic anemia hereditary if caused by medication?
No. Medication-induced aplastic anemia is not inherited. It’s an acquired condition triggered by a drug. However, some people have genetic variations that make them more susceptible to bone marrow damage from certain drugs. Research is ongoing to identify these risk genes through pharmacogenomic testing.
Can you get aplastic anemia from vaccines?
There is no credible evidence linking vaccines to aplastic anemia. Cases reported after vaccination are extremely rare and have not been proven to be caused by the vaccine itself. The benefits of vaccination far outweigh the theoretical risk. If you have concerns, talk to your doctor - but don’t avoid vaccines based on unverified claims.
What should I do if I can’t reach a hematologist right away?
Go to the nearest emergency room. Bring your medication list and recent blood test results if you have them. Tell them you suspect medication-induced bone marrow failure. ER staff are trained to recognize pancytopenia and will order urgent CBC and blood smear tests. Do not wait for a specialist appointment if you have fever, bleeding, or extreme fatigue.
Are there any new tests to detect this earlier?
Yes. The NIH is testing a rapid genetic panel that can identify bone marrow failure within 48 hours by detecting specific immune and stem cell markers. Early results show 92% accuracy. Some hospitals are also piloting AI tools in electronic health records that flag patients on high-risk drugs with early drops in blood counts - before symptoms even appear.
Next Steps: Protect Yourself
If you’re taking any medication on the high-risk list, get a baseline CBC now - even if you feel fine. Ask your doctor about weekly monitoring for the first month. Keep a printed copy of your meds. Download the AAMDS mobile app. Know the warning signs. And if something feels off - don’t wait. Get tested. Your bone marrow can’t speak. But your body can. Listen to it.
malik recoba
November 19, 2025 AT 16:43i started taking carbamazepine last month and i’ve been exhausted since week 2. thought it was just stress or bad sleep. this post scared the hell outta me but also made me realize i need to get my blood checked ASAP. thanks for laying it out so plainly.
Sarbjit Singh
November 19, 2025 AT 23:31bro this is so important!! 😅 i work in a clinic in delhi and saw a guy last month with pancytopenia - he was on Bactrim for a UTI. doc missed it till he was in ICU. pls share this with everyone u know. prevention > cure 🙏
Angela J
November 20, 2025 AT 05:23ok but have you ever wondered if Big Pharma is hiding this? like why isn’t this on every drug label? they know. they always know. i read a whistleblower blog once that said they bury marrow-toxicity data in footnotes. and now they want us to just ‘get tested’? lol. 🤡
Sameer Tawde
November 20, 2025 AT 19:29Stop the med. Get the CBC. Call a hematologist. That’s it. No drama. No waiting. If your body says something’s wrong, trust it. You don’t need a PhD to save your life.
Alex Czartoryski
November 22, 2025 AT 02:42Okay but let’s be real - this is basically a 10-page LinkedIn post dressed up as medical advice. I get it’s important, but the tone is so alarmist. Like, ‘you’re gonna die if you don’t get a CBC in 24 hours’? I’ve been on celecoxib for 5 years and I’m fine. Also, who has time to go to the ER every time they feel tired? 🤦♂️
Victoria Malloy
November 22, 2025 AT 08:51thank you for writing this. i had a cousin who went undiagnosed for months and it broke my heart. i printed this out and gave it to my mom - she’s on phenytoin. small steps, but maybe it’ll help someone.
Gizela Cardoso
November 23, 2025 AT 05:34i downloaded the AAMDS app after reading this. it’s actually kinda nice to log my meds and symptoms. feels like i’m not just ignoring my body anymore.
Andrea Johnston
November 24, 2025 AT 00:38alex is right - this is fearmongering. you’re telling people to stop meds cold turkey? what if they’re on it for seizures? you think the ER is gonna magically fix this? it’s not that simple. also, ‘go to a hematologist yourself’? good luck getting an appointment in Canada without a referral. this post is irresponsible.
Scott Macfadyen
November 25, 2025 AT 06:21andrea, you’re missing the point. it’s not about being irresponsible - it’s about awareness. i had a neighbor die from this. no one knew what was happening until it was too late. yeah, the system sucks. yeah, referrals take forever. but if you’re on carbamazepine and you’re bruising for no reason? you don’t wait for the system to work. you go to the ER. period.