Liver Cirrhosis: Causes, Risks, and Medications That Can Help or Harm
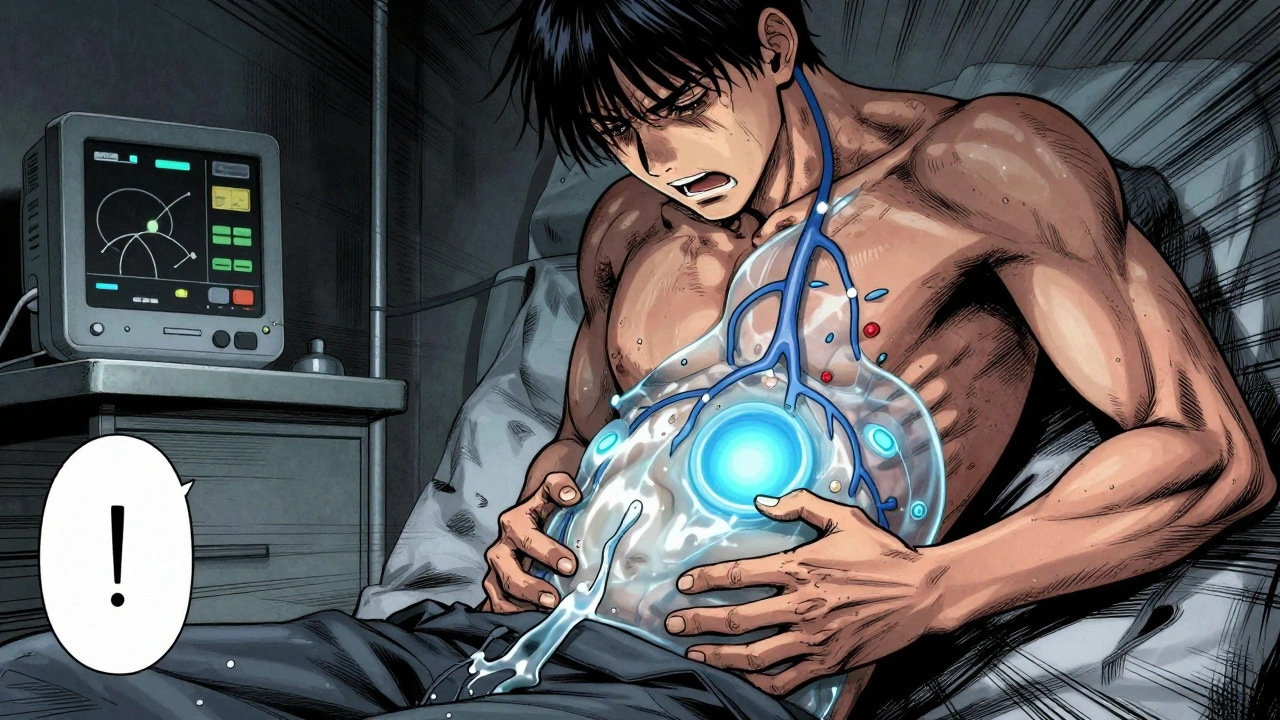
When your liver gets damaged over time, it tries to heal itself—but instead of growing back healthy, it forms scar tissue. This is liver cirrhosis, a late-stage liver disease where healthy tissue is replaced by fibrous scars, blocking blood flow and impairing function. Also known as cirrhosis of the liver, it doesn’t happen overnight. It builds up silently, often for years, before symptoms like fatigue, swelling, or yellow skin show up. The biggest culprits? Long-term alcohol abuse, chronic hepatitis B or C, and non-alcoholic fatty liver disease from obesity or diabetes.
What you take daily can make this worse—or sometimes, even start it. Alcoholic liver disease, a major cause of cirrhosis, happens when drinking over years overwhelms the liver’s ability to process toxins. But it’s not just alcohol. Some painkillers, like high-dose acetaminophen, can trigger liver failure in people with early damage. Even certain antibiotics, antifungals, and herbal supplements like kava or green tea extract have been linked to toxic liver injury. And if you’re on multiple meds—say, for high blood pressure, diabetes, or cholesterol—you might not realize how they stack up. The liver is your body’s filter, and when it’s already scarred, even small doses can become dangerous.
Fatty liver, a condition where fat builds up in liver cells, often without symptoms, can quietly progress to cirrhosis if ignored. It’s not just for heavy drinkers. Over 80 million Americans have it, mostly from eating too much sugar and refined carbs. And here’s the catch: many of the drugs used to treat diabetes and high cholesterol are safe for healthy livers—but risky if cirrhosis is already present. For example, statins are generally okay, but if your liver enzymes are climbing, your doctor needs to know. The same goes for NSAIDs like ibuprofen, which can cause kidney stress and fluid retention in advanced cirrhosis.
Some people think if they stop drinking, their liver will bounce back. It can—if caught early. But once cirrhosis sets in, the damage is mostly permanent. The goal then isn’t reversal, but stopping it from getting worse. That means avoiding alcohol completely, getting tested for hepatitis, managing weight, and reviewing every pill you take—even over-the-counter ones. A single extra dose of Tylenol, or a herbal remedy bought online, could push a fragile liver into failure.
Below, you’ll find real-world guides on how medications can either protect your liver or speed up its decline. From how to spot fake pills that might contain deadly toxins, to understanding why some generics carry hidden risks from inactive ingredients, these posts give you the tools to make smarter choices. You’ll also see how drug interactions, dosage errors, and long-term use of common prescriptions can quietly harm your liver. This isn’t theory. It’s what’s happening in clinics and ERs right now—and you need to know how to protect yourself.