HVPG: What It Is, Why It Matters, and How It Connects to Liver and Portal Hypertension
When doctors need to know how much pressure is building up in the liver’s blood vessels, they turn to HVPG, hepatic venous pressure gradient, a direct measurement of pressure differences in the liver’s venous system. It’s not a test you hear about every day, but for people with cirrhosis, ascites, or bleeding varices, it’s one of the most important numbers in their care. Think of it like checking the water pressure in a clogged pipe—except this pipe is inside your liver, and too much pressure can lead to life-threatening leaks.
HVPG doesn’t just measure pressure—it tells you what’s happening inside the liver. A reading above 5 mmHg is normal. Above 10 mmHg means portal hypertension is present. Above 12 mmHg? That’s when varices are likely forming. And if it hits 16 mmHg or higher, your risk of bleeding skyrockets. This isn’t guesswork. It’s a number that guides whether you need a beta-blocker, a shunt, or even a transplant. It’s also used to track if a treatment is working. If HVPG drops by 20% or more after starting a drug, your chances of surviving the next few years improve dramatically.
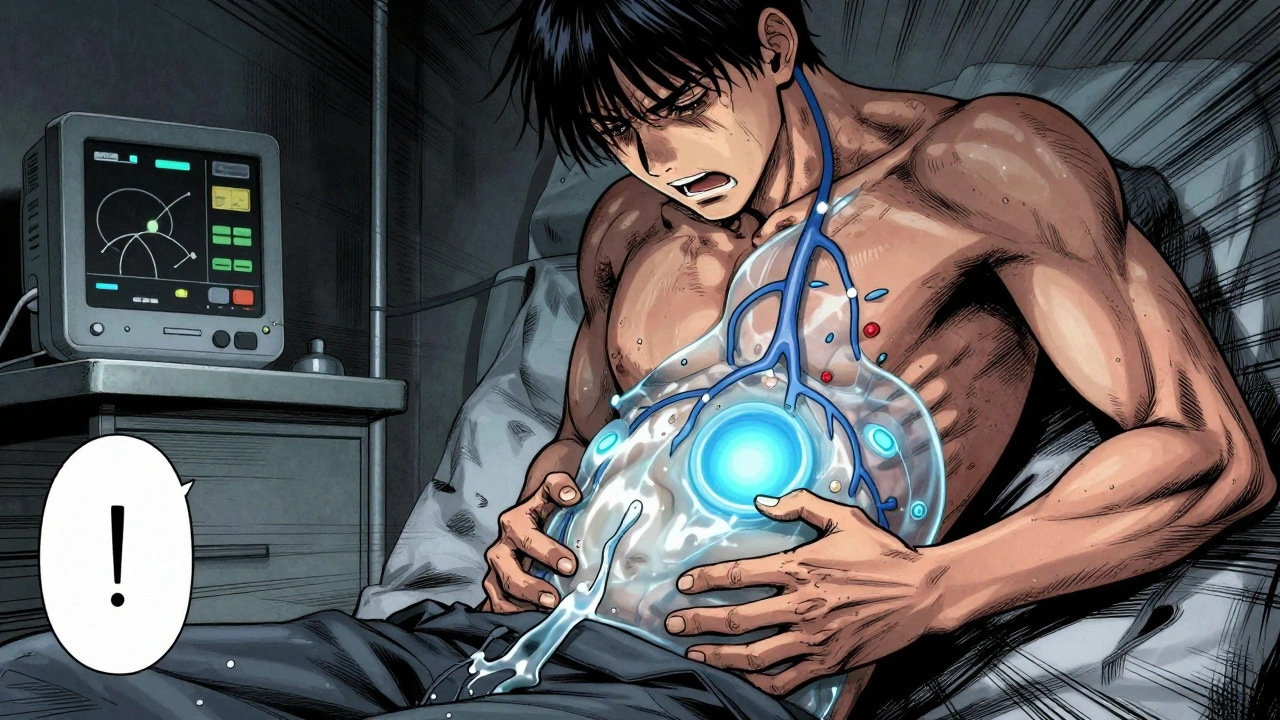
HVPG is tightly linked to other key liver conditions. For example, if you have cirrhosis, scarring of the liver that blocks blood flow and raises pressure in the portal vein, HVPG helps determine how advanced it is. If you’re dealing with ascites, fluid buildup in the abdomen caused by high liver pressure, HVPG tells doctors if diuretics alone will help—or if they need to act faster. And when someone comes in with variceal bleeding, ruptured veins in the esophagus or stomach from portal pressure, HVPG is often checked before and after treatment to see if the bleeding risk has dropped.
It’s not a simple blood test. HVPG requires a catheter to be placed into a liver vein, usually through the neck or groin. It’s done in a hospital, often during an endoscopy or other procedure. But it’s not risky for most people, and the information it gives is unmatched. No imaging scan, no blood marker, no symptom checklist can replace it. That’s why it’s the gold standard—even though it’s not used as often as it should be outside of specialty centers.
What you’ll find in the posts below isn’t just theory. These are real-world stories and guides from people who’ve lived with liver disease, clinicians who’ve used HVPG to save lives, and researchers who’ve proven how this number changes outcomes. You’ll learn how to talk to your doctor about it, what the numbers mean for your treatment, and why some patients get relief while others don’t—even when they’re on the same meds. This isn’t just about a number. It’s about knowing when to push for help, when to question a plan, and when to trust the data.