Double Check Protocol: Why It Saves Lives in Medication Safety
When a nurse hands you a pill, or a pharmacist fills a prescription, there’s a quiet but critical step happening behind the scenes: the double check protocol, a standardized process where two trained professionals independently verify medication details before administration. Also known as two-person verification, it’s not bureaucracy—it’s the last line of defense against deadly mistakes. One wrong dose, one misread label, one mix-up between similar-sounding drugs, and someone could die. The double check protocol exists because humans make errors—and in healthcare, those errors don’t stay small.
This isn’t just about pills. It applies to IV medications, chemotherapy, insulin, blood thinners, and even over-the-counter drugs in high-risk settings. The pharmacy safety, the system of checks and procedures designed to prevent medication errors in dispensing and administration relies on this step. In hospitals, it’s often required for high-alert medications like heparin or morphine. In pharmacies, it’s used when filling prescriptions for elderly patients on five or more drugs. The healthcare errors, preventable mistakes in treatment or medication that cause harm to patients that this protocol stops aren’t rare. Studies show that up to half of all medication errors could be caught by a second set of eyes.
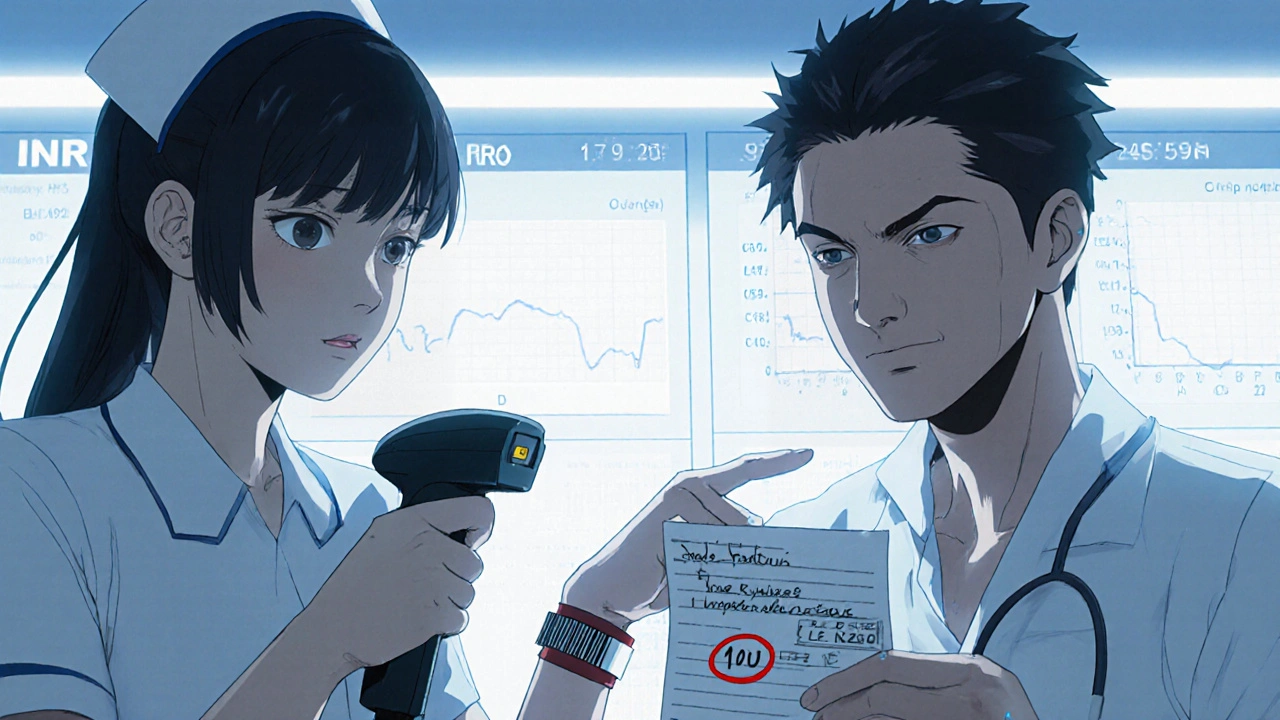
It’s not about distrust. It’s about design. Even the most experienced pharmacist can miss a decimal point or confuse brand names. A tired nurse might overlook a weight-based dosage. A barcode scanner can fail. The drug verification, the process of confirming the right patient, right drug, right dose, right route, and right time before giving medication isn’t just a checklist—it’s a conversation. Two people read the label aloud. They compare it to the order. They check the patient’s allergies. They confirm the route: oral, IV, topical? One person does it. The other confirms it. No shortcuts. No assumptions. This is how you prevent a patient from getting ten times their dose of insulin—or worse, the wrong drug entirely.
You’ll find real examples of this in action across the posts below. From how excipients in generics can trigger reactions if mislabeled, to why warfarin doses need exact verification, to how counterfeit GLP-1 pens slip through without proper checks—every story ties back to one truth: when medication safety fails, it’s rarely because of one big mistake. It’s because the small checks got skipped. The double check protocol isn’t glamorous. It doesn’t make headlines. But it’s the reason millions go home safe every day. Below, you’ll see how this simple step connects to everything from generic drug approval to seizure of fake pills. Because if you don’t verify, you’re not just risking error—you’re risking lives.