Medication errors kill more people in hospitals than car accidents. And a huge chunk of those errors happen when a doctor changes a patient’s dose - and no one double-checks it properly.
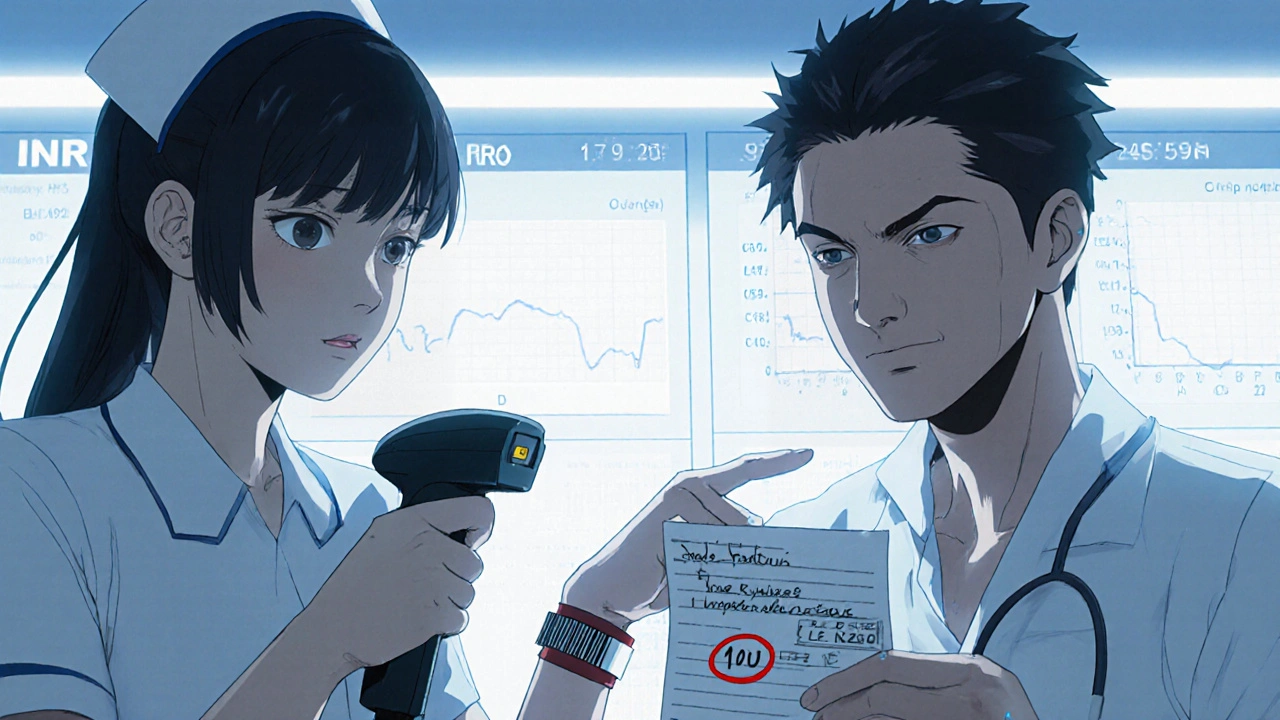
You might think it’s just a matter of reading the prescription correctly. But it’s not. A nurse once almost gave 10 units of insulin instead of 1 unit because the doctor wrote "10U" instead of "1.0U". The double check caught it. That’s not luck. That’s protocol.
Verifying dose changes isn’t about being extra careful. It’s about building layers of safety so one mistake doesn’t become a tragedy. The Institute for Safe Medication Practices (ISMP) says this isn’t optional - it’s a core part of patient safety. And the data backs it up: when verification protocols are followed correctly, medication administration errors drop by nearly 30%.
Why Dose Changes Are the Most Dangerous Moment
Dose changes are high-risk because they’re often urgent, complex, and happen during transitions - like when a patient moves from ICU to a regular floor, or when a new doctor takes over a shift. A 10-fold error in insulin, heparin, or opioids can kill someone in minutes.
Studies show that 65% of serious medication errors linked to death or permanent harm involve miscommunication during dose changes. That’s not just a typo. That’s a broken handoff. A rushed phone call. A scribbled note on a sticky. A tired nurse assuming the dose is right because "it’s what we always give."
High-alert medications - insulin, heparin, opioids, IV potassium, and chemotherapy drugs - are the biggest red flags. These aren’t drugs you guess with. They need systems, not hope.
The Three-Step Verification Process
There’s no magic bullet. But there is a proven method: the 3-step verification process endorsed by ISMP and adopted by top hospitals like Johns Hopkins.
- Independent calculation - Two qualified staff members calculate the dose separately, without talking to each other. For pediatric patients, that means calculating to 0.1 mg/kg. For warfarin, it means checking the INR trend from the last 24 hours. This step takes 2-3 minutes. Don’t skip it.
- Context check - Does the patient’s kidney function allow this dose? Are they on other drugs that interact? Are they fasting? Is this a new diagnosis? This isn’t just paperwork - it’s clinical judgment. Add 1-2 minutes here. Look at the chart. Ask the patient.
- Bedside verification with barcode scanning - Scan the patient’s wristband. Scan the medication. The system should match the dose, route, and time against the electronic order. If it doesn’t, stop. Don’t override it. This step takes 30-60 seconds. But it catches 86% of wrong-drug or wrong-dose errors.
This isn’t bureaucracy. It’s survival. And it works. At one hospital, just adding the context check step reduced insulin errors by 41% in six months.
Barcode Scanning vs. Double Checks - Which One Wins?
People argue about whether technology or human checks are better. The truth? You need both.
Barcode medication administration (BCMA) systems are great at catching the obvious: wrong patient, wrong drug, wrong dose. They prevent 86% of those errors. But they can’t catch everything. If a nurse enters the right concentration but the wrong dose - like 10 mL instead of 1 mL - the system might not flag it. That’s what happened in a 2022 case where a pharmacist almost gave a 10-fold overdose. The barcode scanned fine. The human caught it.
Independent double checks, on the other hand, are better at spotting things machines miss: wrong infusion rate, wrong IV line, misread handwriting, or a dose that looks "off" based on experience. In sepsis simulations, double checks caught 100% of wrong-vial errors. Single checks? Only 54%.
So here’s the rule: Use barcode scanning for drug, patient, and dose match. Use independent double checks for high-alert meds and complex calculations. Don’t pick one. Use them together.
The Communication Breakdown That Kills
Most errors don’t happen because someone’s dumb. They happen because communication breaks down.
That’s why tools like SBAR - Situation, Background, Assessment, Recommendation - are now required in 78% of U.S. hospitals. When a nurse calls a doctor about a dose change, SBAR forces clarity:
- Situation: "Mr. Smith’s systolic BP dropped to 88 after we gave 5 mg IV hydralazine."
- Background: "He’s 72, renal impairment, creatinine 2.1, on lisinopril."
- Assessment: "I think he’s overmedicated. The dose should be cut to 2.5 mg."
- Recommendation: "Can we hold the next dose and reduce to 2.5 mg?"
Studies show SBAR cuts miscommunication errors by 41%. No more "Give him half the usual dose" or "Just reduce it a bit." Clear. Specific. Documented.
And always read back. When a doctor gives a verbal order, the nurse repeats it back word-for-word. "You want 1 unit of insulin?" "Yes." "And you want it subcutaneous now?" "Yes." That’s not annoying. That’s life-saving.
Why Double Checks Fail - And How to Fix Them
Here’s the ugly truth: 92% of hospitals say they do double checks. But only 63% actually do them right.
Why? Time pressure. Staff shortages. Alert fatigue. Nurses told us on forums like Reddit that double checks feel "ritualistic" during busy shifts. One nurse said she skipped them 3 times in one 12-hour shift. Two days later, a patient had a hypoglycemic seizure.
That’s not negligence. That’s a broken system.
The fix? Targeted verification. Don’t double-check everything. Double-check only what’s dangerous.
Johns Hopkins cut their double-check workload by 18% - and still reduced errors - by only requiring them for:
- High-alert medications
- Pediatric doses
- Patients with renal or liver failure
- Any dose change during shift handoff
And they added 15-20 minutes of "safety time" per nurse shift. No tasks. No interruptions. Just time to verify, ask questions, and breathe.
What’s New in 2025
Technology is catching up. Epic’s DoseRange Advisor now uses AI to flag abnormal dose orders before they’re even written - like if a doctor tries to order 500 mg of metformin for a 50 kg patient. It caught 52% of inappropriate orders in a 12-hospital trial.
Mayo Clinic is testing voice recognition tools. Nurses say the dose into a headset, and it auto-populates the chart. Documentation time drops by 65%. No more scribbles. No more misreads.
And blockchain? Still experimental. But it could one day create an unchangeable record of every dose change - who ordered it, who verified it, when, and why.
But none of this matters if the culture doesn’t change. Verification isn’t about checking boxes. It’s about speaking up when something feels wrong. It’s about asking, "Wait - is this right?" It’s about creating an environment where no one feels stupid for double-checking.
What You Can Do Today
You don’t need a new system. You don’t need a budget. You need to start here:
- Stop assuming. If a dose looks odd - even if it’s "standard" - pause. Verify.
- Use SBAR. Every time you communicate a dose change. No exceptions.
- Scan. Always. Even if you’re in a rush. The barcode is your last line of defense.
- Double-check high-alert meds. Insulin. Heparin. Opioids. Never skip this.
- Document everything. Time. Names. Calculations. INR. Renal function. If it’s not written, it didn’t happen.
And if you’re in charge? Protect your staff’s time. Give them safety time. Train them with simulations. Reward them for speaking up. The best verification system in the world fails if people are too tired or scared to use it.
Medication safety isn’t about technology. It’s about people. And when people are supported, errors drop. Patients live. That’s the only metric that matters.
Deepak Mishra
November 16, 2025 AT 08:53OMG this is SO TRUE!!! I work in a hospital in Delhi and last week a nurse almost gave a patient 10x insulin because the doc wrote "10U"!!! 😱 I screamed so loud the whole unit turned around... we all need to stop being lazy!!! 🙏💉
Rachel Wusowicz
November 17, 2025 AT 05:46Let’s be real-this whole ‘verification protocol’ is just corporate theater. The real problem? Hospitals are run like factories now. Nurses are treated like disposable widgets. The barcode scanners? They’re a distraction. The AI tools? Just more data for the insurance companies to deny care later. And don’t even get me started on how they ‘reward’ staff for speaking up… right after they get written up for ‘disrupting workflow.’ This isn’t safety-it’s a PR stunt wrapped in a PowerPoint. They’ll never fix the system until they stop treating people like machines.
Diane Tomaszewski
November 17, 2025 AT 22:36It’s simple really. If you’re not sure, stop. Ask. Check. Don’t rush. People die when we don’t. That’s it.
Teresa Smith
November 19, 2025 AT 12:19As someone who has trained new nurses for over a decade, I’ve seen the erosion of safety culture firsthand. The 3-step verification process isn’t bureaucracy-it’s the last human barrier between a patient and irreversible harm. What’s alarming isn’t that errors happen, but that we’ve normalized the risk. We call it ‘efficiency’ when we skip steps, but it’s really just moral fatigue. The fix isn’t more tech-it’s more dignity. Give nurses time. Respect their judgment. Let them pause without fear. When we treat caregivers as professionals instead of cogs, the protocols follow naturally.
Dan Angles
November 20, 2025 AT 05:24While the proposed verification framework is commendable, its implementation remains contingent upon institutional compliance and workforce capacity. It is imperative that administrative leadership not only endorse but actively resource these protocols through staffing augmentation, dedicated safety time, and mandatory simulation-based competency assessments. Without structural investment, even the most evidence-based practices remain aspirational. The data are unequivocal; the ethical imperative is non-negotiable.
David Rooksby
November 20, 2025 AT 06:01Okay but let’s be honest here-how many of these ‘verified’ doses are still wrong because the person doing the double-check is just as tired as the first one? I’ve seen it a hundred times. Nurse A writes down the dose, Nurse B nods and says ‘looks good’ without even looking at the chart. It’s a ritual. A checkbox. A performance. And the system rewards it. Meanwhile, the AI that flags weird doses? That’s the only thing that’s actually saving lives. The rest is theater. And don’t even get me started on SBAR-half the nurses I work with don’t even know what the ‘B’ stands for. They just say ‘patient bad, fix it’ and hang up. This whole thing is a house of cards built on good intentions and bad sleep.
Melanie Taylor
November 20, 2025 AT 10:30As a nurse from rural Texas who moved to NYC last year-I can tell you, the culture difference is wild. Back home, everyone just ‘knew’ the doses. Here? We scan, we double-check, we use SBAR, we have safety time… and yeah, it feels slow at first. But I had a patient last week who would’ve died if I’d just ‘assumed’ the insulin dose. Now I don’t care how busy I am-I pause. I breathe. I check. 🙏❤️🇺🇸🇳🇾🇨🇦
ZAK SCHADER
November 20, 2025 AT 14:37Why are we wasting time on this? In America we have the best medical tech in the world. All this double-checking is just European bureaucracy creeping in. We don’t need 15-minute safety pauses-we need more nurses who can think on their feet. Stop coddling people. If you can’t handle the job, go work at a Starbucks. This isn’t daycare. It’s medicine. And if you’re too tired to give the right dose? Maybe you shouldn’t be on shift.