Bioequivalence: What It Means for Generic Drugs and Your Health
When you pick up a generic pill, you’re trusting that it does the same job as the brand-name version. That trust comes down to bioequivalence, the scientific standard that proves two drug products deliver the same amount of active ingredient at the same rate in your body. Also known as pharmaceutical equivalence, it’s not just a regulatory checkbox—it’s what keeps your treatment safe and predictable. If a generic isn’t bioequivalent, it might not work at all—or worse, it could cause side effects you didn’t expect.
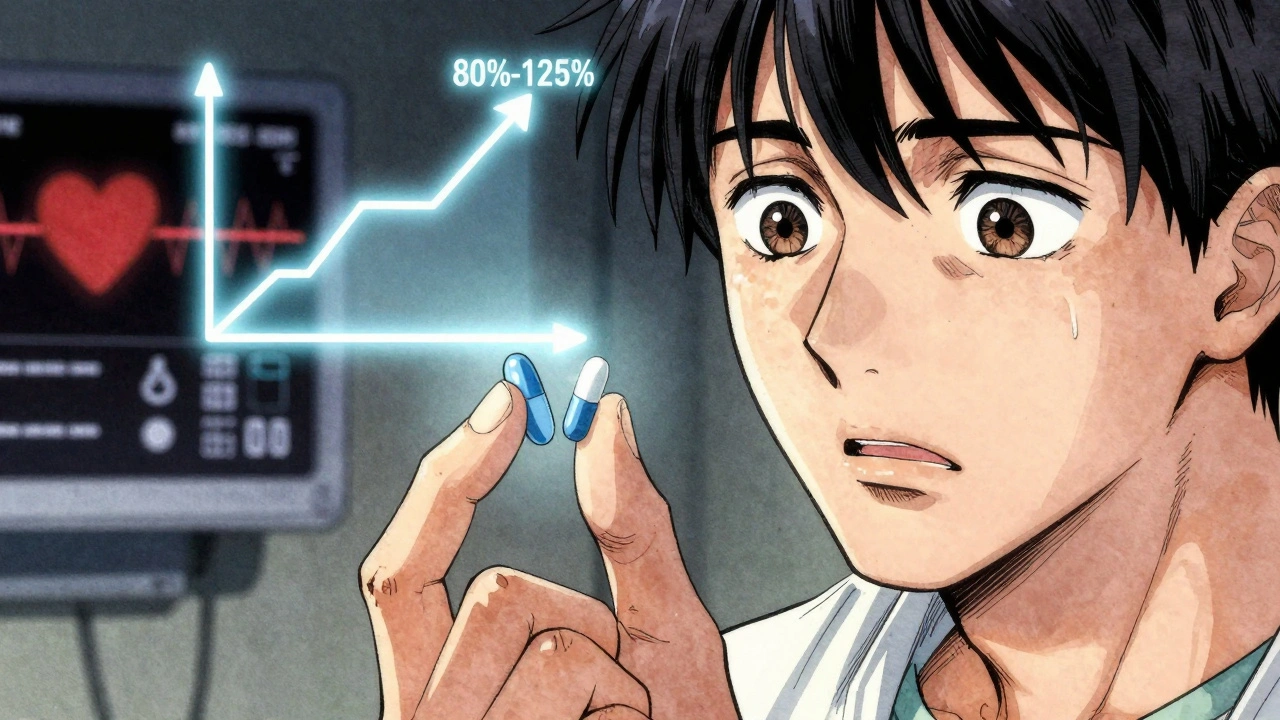
Bioequivalence isn’t about the pill looking the same. It’s about what happens inside you. The drug must be absorbed into your bloodstream at the same speed and to the same level as the original. That’s why regulators like the FDA require strict testing—usually with healthy volunteers who take both versions and have their blood drawn over time. If the curves of drug levels match within 80–125%, it’s approved. This applies to every generic you take: from blood pressure pills to antibiotics. But here’s the catch: bioequivalence doesn’t guarantee identical side effects. That’s because excipients, the inactive ingredients like fillers and dyes. Also known as inactive ingredients, it can vary between brands. A generic might use lactose instead of cornstarch, and if you’re sensitive, that’s when problems start—even if the active drug is perfectly matched.
That’s why some people swear their brand-name drug works better. It’s not always placebo. Sometimes, it’s the formulation, how the drug is built inside the pill—its coating, release speed, or how it dissolves. Also known as drug delivery system, it that makes the difference. For drugs with a narrow therapeutic window—like warfarin, lithium, or seizure meds—even tiny changes in absorption can throw off your dose. That’s why doctors sometimes stick with brand names for these. But for most people, generics are just as safe and effective. The real risk isn’t bioequivalence itself—it’s buying fake or unregulated generics online. We’ve seen cases where counterfeit pills labeled as generics contain nothing, wrong doses, or toxic chemicals. That’s why verifying your pharmacy matters more than ever.
What you’ll find in these posts isn’t just theory. It’s real stories: people reacting to fillers in generics, confusion over switching meds, and how even small changes in drug delivery can affect your health. You’ll read about why some people can’t tolerate certain generics, how to spot if your medication isn’t working like it should, and what questions to ask your pharmacist before you refill. This isn’t about choosing between brand and generic—it’s about understanding what’s really in your pill, how it gets to your bloodstream, and how to make sure it works for you—every time.