Antibiotic Side Effects: What You Need to Know Before Taking Them
When you take an antibiotic, a medicine designed to kill or slow down harmful bacteria. Also known as antibacterial agents, they’re one of the most common drugs prescribed worldwide—but they don’t just target bad bacteria. They also hit the good ones, and that’s where most side effects start.
Not all antibiotics cause the same problems. Some, like cephalexin, a common penicillin-like drug used for skin and respiratory infections, often lead to nausea or diarrhea. Others, like fluoroquinolones, a class including ciprofloxacin and levofloxacin, used for UTIs and pneumonia, can trigger nerve damage, tendon ruptures, or even long-term joint pain. Then there’s clindamycin, a strong antibiotic often used for acne or dental infections, which carries a rare but deadly risk of C. diff colitis—a severe gut infection that can require surgery. These aren’t rare outliers. They’re documented risks you need to know before swallowing that pill.
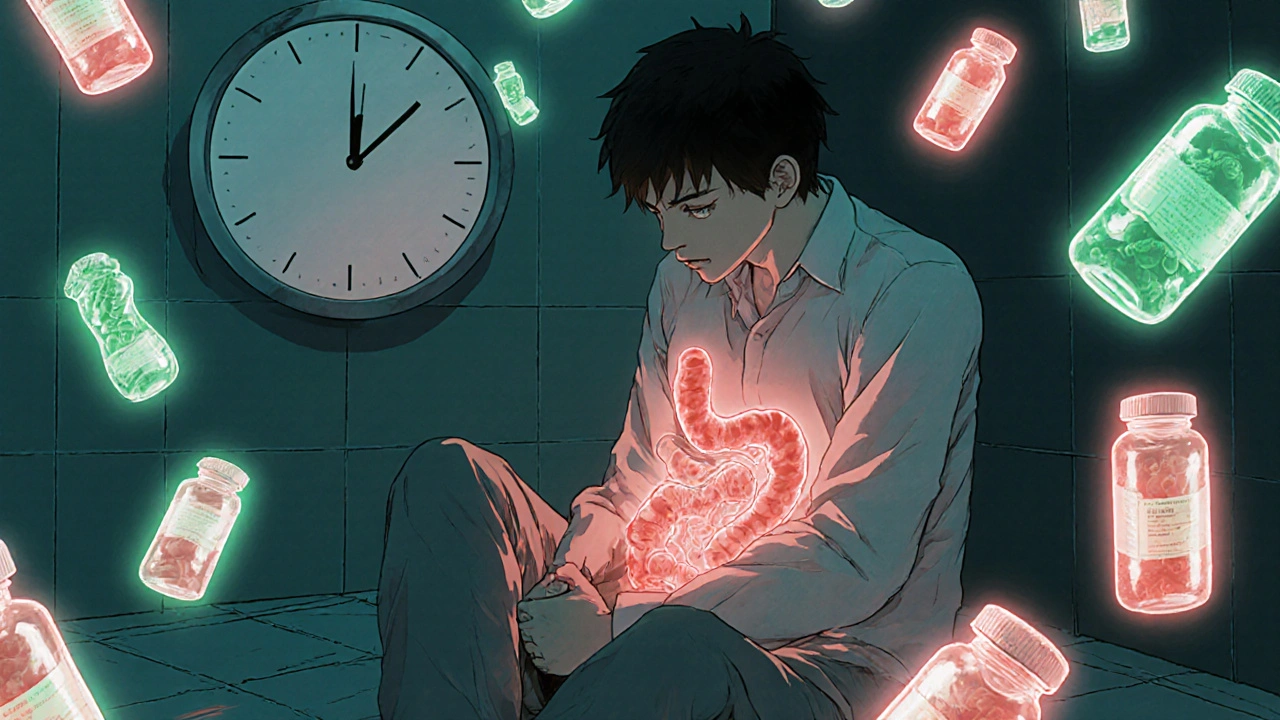
One of the biggest hidden issues? Your gut. Antibiotics wipe out trillions of helpful bacteria in your intestines, which can throw off digestion, weaken your immune system, and even affect your mood. Studies show that even a single course can change your microbiome for months. And it’s not just about diarrhea. Some people develop yeast infections, rashes, or extreme fatigue weeks after finishing a round. If you’ve ever felt "off" long after an antibiotic course ended, it might not be in your head—it’s in your gut.
Another risk most people ignore? Drug interactions. Antibiotics like doxycycline, a tetracycline-class drug used for acne and Lyme disease, lose effectiveness if taken with dairy or antacids. Others, like azithromycin, a macrolide antibiotic often used for respiratory infections, can interfere with heart rhythm medications. Even something as simple as ibuprofen or birth control pills can react badly. You can’t just grab an antibiotic and go—knowing what else you’re taking matters as much as the dose.
And then there’s the bigger picture: antibiotic resistance. Every time you take one unnecessarily, you’re helping superbugs evolve. That’s why doctors now avoid prescribing them for colds, flu, or most sore throats—even if you’re desperate for relief. But if you’re prescribed one, don’t skip doses or stop early. That’s how resistant strains survive. Completing the full course isn’t about being obedient—it’s about survival.
What you’ll find in the posts below are real-world cases and comparisons that cut through the noise. You’ll see how cefixime stacks up against amoxicillin, why nitrofurantoin works better for some UTIs, and how excipients in generic versions can trigger reactions you never expected. You’ll learn how to spot early signs of serious reactions like blood disorders or liver damage. These aren’t theory pages—they’re based on actual patient reports, clinical data, and pharmacy warnings. If you’ve ever wondered why you felt awful after an antibiotic, or if your doctor dismissed your concerns, you’ll find answers here.