Probiotic Timing & Strain Calculator
Personalize Your Probiotic Plan
When you’re on antibiotics, your body is fighting an infection-but your gut is paying the price. Antibiotics don’t just kill bad bacteria; they wipe out the good ones too. The result? Diarrhea, bloating, nausea, and in some cases, a dangerous Clostridioides difficile infection. Many people assume this is just a side effect you have to live with. But what if you could reduce those symptoms-and protect your gut-without stopping your treatment?
The answer isn’t magic. It’s probiotics. Not all of them, though. Not any random supplement from the shelf. The right strains, taken at the right time, can cut your risk of antibiotic-associated diarrhea by up to two-thirds. But get it wrong, and you might do more harm than good. This isn’t about popping a pill and hoping for the best. It’s about knowing which strains work, when to take them, and who should avoid them entirely.
Why Antibiotics Mess Up Your Gut
Antibiotics are broad-spectrum weapons. They don’t pick and choose. Whether you’re taking amoxicillin for a sinus infection or clindamycin for a skin abscess, these drugs flood your system and wipe out bacteria indiscriminately. Your gut holds trillions of microbes-bacteria, fungi, viruses-that help digest food, train your immune system, and even influence your mood. When antibiotics hit, up to 30% of those good bacteria can vanish within days.
The fallout? Diarrhea. Not just any diarrhea-antibiotic-associated diarrhea (AAD). About 20% of adults on antibiotics get it. For older adults or those on broad-spectrum drugs like piperacillin-tazobactam, the rate jumps to 40%. In severe cases, the gut lining gets stripped bare, letting Clostridioides difficile (C. diff) take over. C. diff causes violent diarrhea, fever, and can lead to colon surgery or death. It’s not rare. In the U.S. alone, over 500,000 cases happen each year.
Probiotics don’t stop antibiotics from working. They don’t interfere with the drug’s ability to kill the infection. What they do is fill the gaps left behind-replacing lost bacteria, crowding out harmful ones, and calming inflammation in the gut lining. It’s like sending in a cleanup crew while the main repair team is still at work.
The Probiotics That Actually Work
Not all probiotics are created equal. You can’t just grab any bottle labeled "probiotic" and expect results. The science is clear: only specific strains have been proven to help during antibiotic use.
The two most studied and effective strains are:
- Lactobacillus rhamnosus GG-This strain has been tested in over 20 clinical trials. It reduces AAD risk by 55% on average. It’s the main ingredient in Culturelle, a widely available supplement.
- Saccharomyces boulardii CNCM I-745-This isn’t a bacterium; it’s a yeast. It’s especially good at preventing C. diff. Studies show it cuts C. diff risk by 66% when taken with antibiotics. It’s sold under brands like Florastor.
Other strains like Bifidobacterium lactis and Lactobacillus acidophilus show some benefit, but the evidence isn’t as strong. If you’re choosing a supplement, look for one that lists these exact strain names on the label-not just "Lactobacillus" or "probiotic blend."
And dosage matters. Most effective studies use between 10 billion and 50 billion colony-forming units (CFUs) per day. That’s usually one to two capsules daily. Lower doses often don’t work. Higher doses don’t necessarily work better-just more expensive.
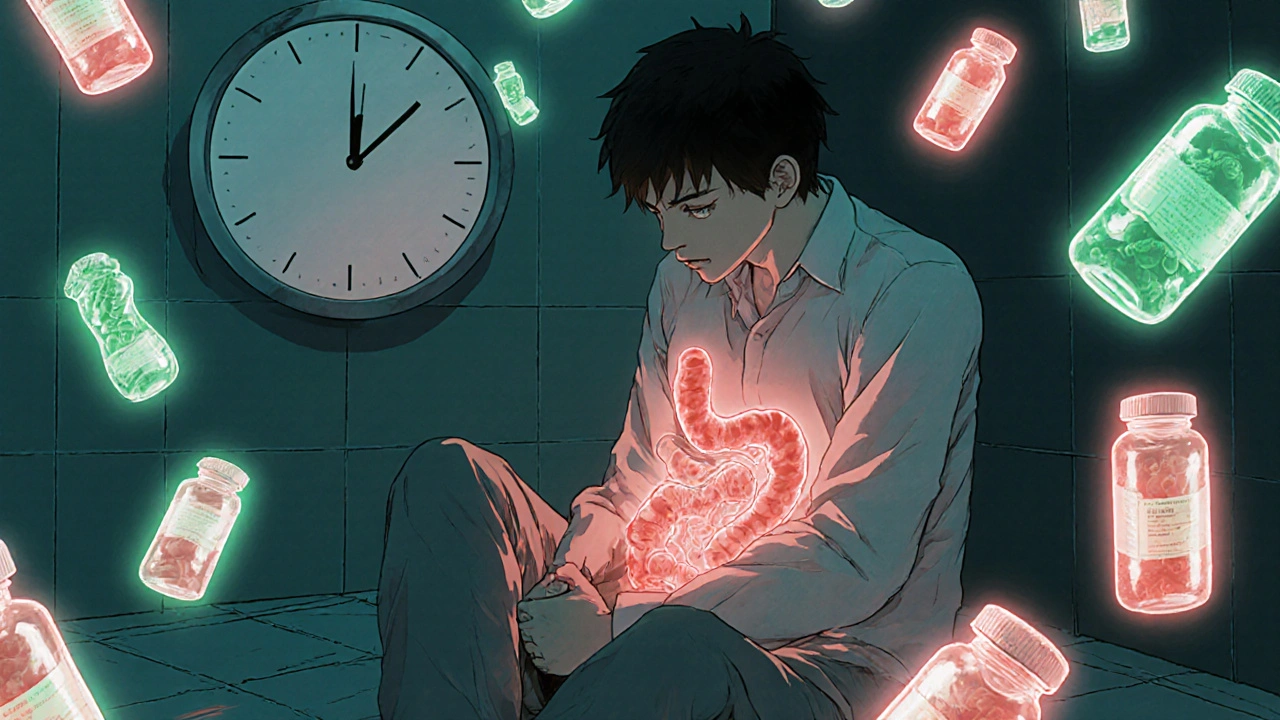
When and How to Take Them
Timing is everything. If you take your probiotic at the same time as your antibiotic, the antibiotic will kill the probiotic bacteria before they can do anything. That’s why you need to space them out.
The best practice? Take your probiotic 2 hours after your antibiotic dose. This gives the antibiotic time to work and reduces direct contact with the probiotic. If you take antibiotics three times a day, take your probiotic with your midday or evening meal. If you take it once a day, take it after that dose.
Don’t stop the probiotic when your antibiotic course ends. Keep taking it for another week or two. Your gut needs time to rebuild. Studies show that continuing probiotics after antibiotics leads to faster microbiome recovery and lower long-term diarrhea risk.
Some people swear by refrigerated probiotics. There’s a reason: they’re more likely to survive. A 2022 ConsumerLab test found that 78% of refrigerated probiotics contained the labeled number of live cultures. Shelf-stable ones? Only 62%. If you’re serious about results, choose refrigerated. If that’s not possible, look for products with enteric coatings or spore-forming strains like Bacillus coagulans, which survive stomach acid better.
The Risks You Can’t Ignore
Probiotics are generally safe-but not for everyone.
If you’re immunocompromised-on chemotherapy, taking high-dose steroids, have HIV with low CD4 counts, or have a central line-you’re at risk. There are documented cases of people developing bloodstream infections from probiotics. Between 2010 and 2020, 12 such cases were reported in medical journals. One Reddit user, u/ChemoPatient, shared how they developed bacteremia after taking probiotics during neutropenia. It’s rare, but it’s real.
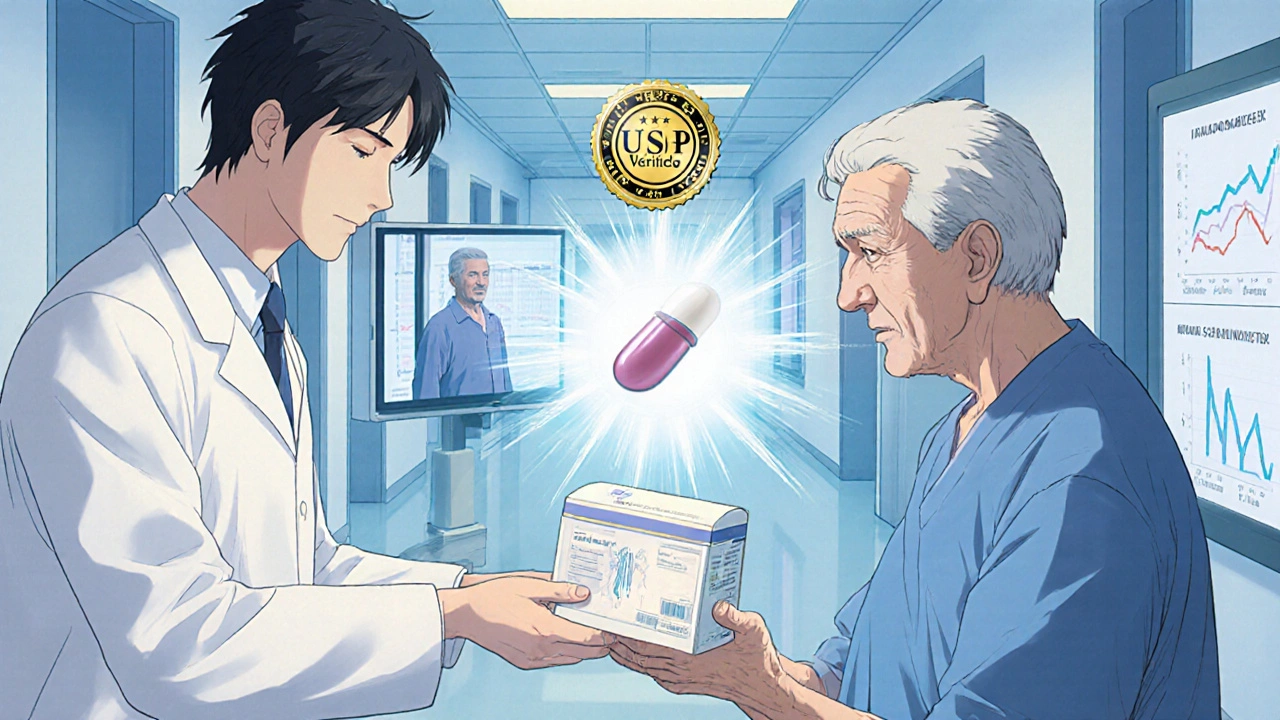
Another concern? Antibiotic resistance genes. A 2025 study in mSphere found that 38% of commercial probiotic products carry genes that make bacteria resistant to common antibiotics like tetracycline and macrolides. These genes can potentially transfer to harmful gut bacteria. The FDA is now requiring manufacturers to screen for these genes, but it’s not mandatory yet. If you’re concerned, look for USP Verified products-they’re tested for purity and label accuracy.
Then there’s the controversial 2018 Cell study. In a small group of 21 healthy people, researchers found that those who took a multi-strain probiotic after antibiotics had a slower return to their original gut microbiome than those who didn’t take any. It was surprising. But since then, larger studies haven’t confirmed it. The scientific consensus still leans toward benefit over risk-for most people.
What the Experts Say
There’s no universal agreement among doctors. The Infectious Diseases Society of America (IDSA) recommends probiotics for high-risk patients to prevent C. diff. The American Gastroenterological Association (AGA) says no-because product quality is too inconsistent.
But here’s what the data shows: if you’re a healthy adult taking antibiotics for a common infection, the benefits outweigh the risks. A 2022 review of 29 studies found that probiotics reduced C. diff risk by two-thirds. Another meta-analysis of 8,670 patients showed a 42% drop in diarrhea. That’s not a small effect. That’s life-changing for someone who’s spent days in the bathroom.
Dr. Elisa Marroquin, lead author of the 2022 review, put it simply: "When participants take antibiotics, we see several consistent changes in bacterial species. But when treatment was combined with probiotics, the majority of those changes were less pronounced and some changes were completely prevented."
Most primary care doctors in the U.S. now recommend probiotics for AAD prevention-62% do, according to a 2022 Medscape survey. But only 28% do it routinely. Why? Because insurance won’t cover it. Most probiotics cost $20 to $45 a month. That’s out-of-pocket. And many doctors don’t know which brand to recommend.
Real People, Real Results
Online reviews tell the same story. On Amazon, probiotics for antibiotic use average 4.1 out of 5 stars. On Reddit, threads in r/Probiotics and r/GutHealth are full of posts like:
"Took Culturelle with my 10-day amoxicillin course. No diarrhea this time-unlike last year when I was stuck in the bathroom for days."
But there are also failures:
"Spent $35 on Garden of Life. Still got C. diff after clindamycin."
What’s the difference? The first person took a proven strain (L. rhamnosus GG). The second used a brand with unknown strains and no clinical backing. It’s not that probiotics don’t work. It’s that most people don’t know which ones to pick.
What to Do Next
If you’re about to start antibiotics:
- Ask your doctor if probiotics are right for you. Especially if you’re over 65, have had C. diff before, or are immunocompromised.
- If they say yes, ask for a specific strain: Lactobacillus rhamnosus GG or Saccharomyces boulardii CNCM I-745.
- Choose a product with at least 10 billion CFUs per dose. Look for refrigerated options or USP Verified labels.
- Take it 2 hours after your antibiotic. Don’t mix them.
- Keep taking it for 1-2 weeks after your antibiotic course ends.
If you’re already on antibiotics and didn’t start probiotics? It’s not too late. Start today. Even if you’re halfway through your course, you can still reduce your risk of diarrhea.
And if you’re immunocompromised? Skip probiotics. Talk to your doctor about alternatives like fecal microbiota transplantation (FMT) if you’re at high risk for C. diff. FMT is more effective but carries higher risks and isn’t available everywhere.
What’s Coming Next
The future of probiotics isn’t random blends. It’s precision. Companies are developing next-generation probiotics like VE303-a defined mix of 8 bacterial strains designed specifically to prevent C. diff after antibiotics. Phase 2 trials showed a 76% reduction in infection. These aren’t in stores yet, but they’re coming.
Regulation is catching up too. The FDA’s new draft guidelines will force manufacturers to test for antibiotic resistance genes. That’s a big step. Right now, you’re buying a product that might contain hidden genes that could make future infections harder to treat. That’s not just a risk to you-it’s a public health issue.
For now, the best tool you have is simple: know your strain, time your dose, and choose quality. Probiotics aren’t a cure-all. But for millions of people taking antibiotics every year, they’re the most effective, low-risk way to protect their gut-and their quality of life.
Joseph Peel
November 18, 2025 AT 18:26Lactobacillus rhamnosus GG and Saccharomyces boulardii CNCM I-745 are the only strains with consistent, high-quality clinical evidence for reducing antibiotic-associated diarrhea. Anything else is marketing. Look for the strain designation on the label, not vague terms like "probiotic blend." If it doesn’t specify, it’s not worth your money.
Kelsey Robertson
November 19, 2025 AT 09:06Probiotics? Really? You’re telling me we can fix the damage of industrial medicine with a $40 supplement? The gut isn’t a garden you can replant with a few lactic acid bacteria. The microbiome is a complex, dynamic ecosystem-reducing it to "good vs. bad" is medieval thinking. And don’t even get me started on the antibiotic resistance genes hidden in these products-regulation? Please. The FDA is asleep at the wheel.
Joseph Townsend
November 19, 2025 AT 11:25Bro. I took amoxicillin last year and thought I was gonna die from the diarrhea. Then I tried Culturelle-like, literally, day two, I felt like a human again. No more bathroom marathons. No more fear of leaving the house. I even started sleeping through the night. It wasn’t magic-it was science. And now I’m telling everyone. Probiotics aren’t optional. They’re essential. If you’re on antibiotics and not taking them, you’re basically letting your gut get mugged.
Bill Machi
November 20, 2025 AT 07:04This is a textbook example of why American healthcare has become a commodity-driven circus. Instead of investing in proper infection control, we hand out probiotic pills like candy. Meanwhile, our hospitals are breeding grounds for C. diff. The real solution is antibiotic stewardship-not popping capsules. And why should a working-class American pay $35 a month out of pocket for something that should be covered? This isn’t health. It’s corporate exploitation dressed up as wellness.
Elia DOnald Maluleke
November 21, 2025 AT 18:33In the grand architecture of human biology, the gut is not merely an organ-it is the silent cathedral where the symphony of life is conducted. To disrupt its delicate harmonies with broad-spectrum antibiotics, then attempt to restore balance with commercial probiotics, is to place a Band-Aid on a ruptured artery. The science, though promising, remains nascent. We must proceed with humility, not hype.
satya pradeep
November 23, 2025 AT 13:35Bro i took this garden of life stuff after antibiotics and still got c diff 😭 why? i spent 35 bucks on it too. now im on vanco and my whole life is ruined. the real answer? just dont take antibiotics unless you really need them. and if you do, go for narrow spectrum. probiotics are a scam for people who wanna feel like they're doing something.
Prem Hungry
November 25, 2025 AT 02:58Dear friend, your body is a temple, and your gut is its most sacred space. When antibiotics invade, they do not discriminate. But you, with wisdom, can protect what is holy. Choose L. rhamnosus GG. Take it two hours after your dose. Continue for two weeks. Do not skip. Your future self will thank you. You are not alone. We walk this path together.
Leslie Douglas-Churchwell
November 26, 2025 AT 19:44Probiotics are just the gateway drug to the Big Pharma gut manipulation agenda. 🤫 Did you know that 92% of these "clinical studies" are funded by supplement companies? And those "antibiotic resistance genes"? They’re not accidents-they’re engineered. The FDA’s draft guidelines? A PR stunt. Real health is fasting, fermented foods, and avoiding processed everything. Stick to sauerkraut. 🥬✨
shubham seth
November 27, 2025 AT 13:12Let’s be real-this whole probiotic thing is a billionaire’s fantasy. You think your $40 bottle of Culturelle is going to fix what your 10-day course of amoxicillin shattered? Nah. You’re just feeding a trillion-dollar industry that profits from your fear. Meanwhile, your microbiome is still a warzone. And guess what? You’re not even getting the strains you paid for. Most products are mislabeled. This isn’t medicine. It’s placebo capitalism.
Kathryn Ware
November 28, 2025 AT 17:58I’ve been a nurse for 18 years and I’ve seen patients go from bedridden with C. diff to walking again after starting Saccharomyces boulardii. It’s not magic, but it’s powerful. I always recommend it to my patients over 65 or those with a history of diarrhea. I even keep a list of USP-verified brands on my clipboard. The key is consistency and quality. And yes, refrigerated is worth the extra effort. Your gut will thank you. You’re not just preventing diarrhea-you’re protecting your long-term health. Trust the science. And if you’re unsure, ask your pharmacist-they know more than you think.
kora ortiz
November 29, 2025 AT 13:56Start today. No excuses. Two hours after your antibiotic. Keep going for two weeks. That’s it. Your gut will recover faster. You’ll feel better. You’ll sleep better. You’ll stop dreading the bathroom. Simple. Effective. Done.
Jeremy Hernandez
November 29, 2025 AT 21:40Yeah right. Probiotics. Like that’s gonna fix what Big Pharma and the USDA did to your gut. You think a capsule is gonna undo glyphosate, high-fructose corn syrup, and 15 years of antibiotics? Please. You’re just paying to feel better while your microbiome turns into a radioactive wasteland. And don’t even get me started on how they’re selling this as a fix instead of asking why we’re on antibiotics in the first place. This is the definition of treating symptoms, not causes.
Tarryne Rolle
November 30, 2025 AT 18:42Probiotics are the modern equivalent of bloodletting. We don’t understand the microbiome well enough to prescribe specific strains with confidence. The 2018 Cell study was ignored because it contradicted the narrative. And now we’re pushing supplements on healthy people like they’re vitamins. We’re not healers-we’re alchemists pretending to be scientists. The real answer? Let the body heal itself. Intervention is arrogance dressed as care.
Kyle Swatt
December 2, 2025 AT 17:40I used to think probiotics were a scam too. Then I got hospitalized after a course of clindamycin. I was dehydrated, weak, and scared. The doctor said, "Try Florastor." I did. Two days later, I was eating again. Not cured-but alive. I’m not saying it’s perfect. I’m saying it’s real. For some people, it’s the line between suffering and survival. Don’t dismiss it because it’s not a cure-all. Sometimes, the smallest thing keeps you from falling off the cliff.
Deb McLachlin
December 2, 2025 AT 18:36The distinction between strain-specific efficacy and generic probiotic marketing is critical. As a researcher, I emphasize the importance of clinical trial reproducibility. The strains cited-L. rhamnosus GG and S. boulardii CNCM I-745-are the only ones with randomized, double-blind, placebo-controlled data supporting their use in antibiotic-associated diarrhea. Other formulations lack this rigor. Consumers must be educated to read labels with precision. The burden of proof lies with manufacturers, not the public.