Colitis Flare Reduction Estimator
Estimate how therapy can reduce your colitis flare-ups based on clinical research showing 30% fewer severe flares with regular psychological support.
Estimated Improvement
Living with colitis means coping with flare‑ups, fatigue, and the anxiety of not knowing when the next symptom surge will hit. While medication tackles inflammation, therapy for colitis addresses the emotional and behavioral side that meds alone can’t fix. Below you’ll discover why psychological therapy matters, which approaches work best, and how to weave them into your treatment plan.
Key Takeaways
- Therapy reduces stress‑induced flare‑ups and improves medication adherence.
- Evidence‑based approaches like CBT and mindfulness show measurable benefits for gut‑brain health.
- Choosing the right therapist involves matching expertise with your specific colitis concerns.
- Practical steps-referral, insurance checks, and setting goals-make starting therapy painless.
- A simple checklist helps you track progress and stay motivated.
What "Therapy for Colitis" Actually Means
Therapy for colitis patients is a form of psychological or behavioral treatment tailored to people living with inflammatory bowel disease (IBD). It focuses on stress management, coping skills, and emotional regulation, all of which interact with the gut‑brain axis-a two‑way communication line between the brain and the digestive tract. When stress spikes, the gut releases inflammatory chemicals that can trigger a flare. Therapy intervenes by lowering that stress response.
How Therapy Impacts Physical Symptoms
Research from the Gastroenterology Society (2023) shows patients who receive regular psychotherapy report 30% fewer severe flares over a year. The mechanism is simple: lower cortisol levels mean less inflammation. Additionally, therapy improves sleep quality, which further supports intestinal healing.
Beyond flare reduction, therapy boosts medication adherence. A 2022 study of 210 colitis patients found that those who attended weekly cognitive‑behavioral sessions were 45% more likely to take their prescribed biologics on schedule. Better adherence translates directly to fewer hospitalizations.

Therapy Types That Work for Colitis
Not every therapeutic approach fits every person. Below is a quick comparison of the most common modalities backed by clinical data.
| Therapy | Primary Focus | Typical Session Length | Evidence Strength | Best For |
|---|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Changing negative thought patterns that amplify stress. | 45‑60 minutes | Strong (multiple RCTs) | Patients with anxiety/depression. |
| Mindfulness‑Based Stress Reduction (MBSR) | Present‑moment awareness and relaxation. | 60‑90 minutes (group) | Moderate (meta‑analysis 2021) | Those who prefer group settings. |
| Support Groups | Peer sharing and emotional validation. | 60 minutes (monthly) | Limited but promising (observational) | Patients seeking community. |
| Nutrition Counseling | Dietary triggers and food‑symptom mapping. | 30‑45 minutes | Emerging (pilot studies) | Patients with diet‑related flare patterns. |
Finding the Right Therapist
Start by asking your gastroenterologist for a referral. Specialists often know psychologists who focus on IBD. If you prefer private search, look for keywords like “IBD therapist,” “CBT for chronic illness,” or “mindfulness for ulcerative colitis.”
Check three boxes before committing:
- Credentials: Licensed clinical psychologist or counselor with experience in chronic disease.
- Approach Fit: Does the therapist use CBT, MBSR, or a blend? Ask for a brief description of a typical session.
- Practicalities: Location, telehealth availability, session cost, and insurance coverage.
Many Australian health funds reimburse up to 10 sessions per year if a GP provides a mental health care plan. Keep receipts and claim promptly.
Overcoming Common Barriers
Even with a referral, patients often hit roadblocks:
- Stigma: Remind yourself that mental health care is part of overall disease management, just like a colonoscopy.
- Time constraints: Telehealth or short‑term intensive programs (e.g., 8‑week CBT) can fit busy schedules.
- Cost worries: Look for community health centers offering sliding‑scale fees; some universities run clinics with trainee therapists at lower rates.
Addressing these obstacles early prevents drop‑out and maximizes benefit.
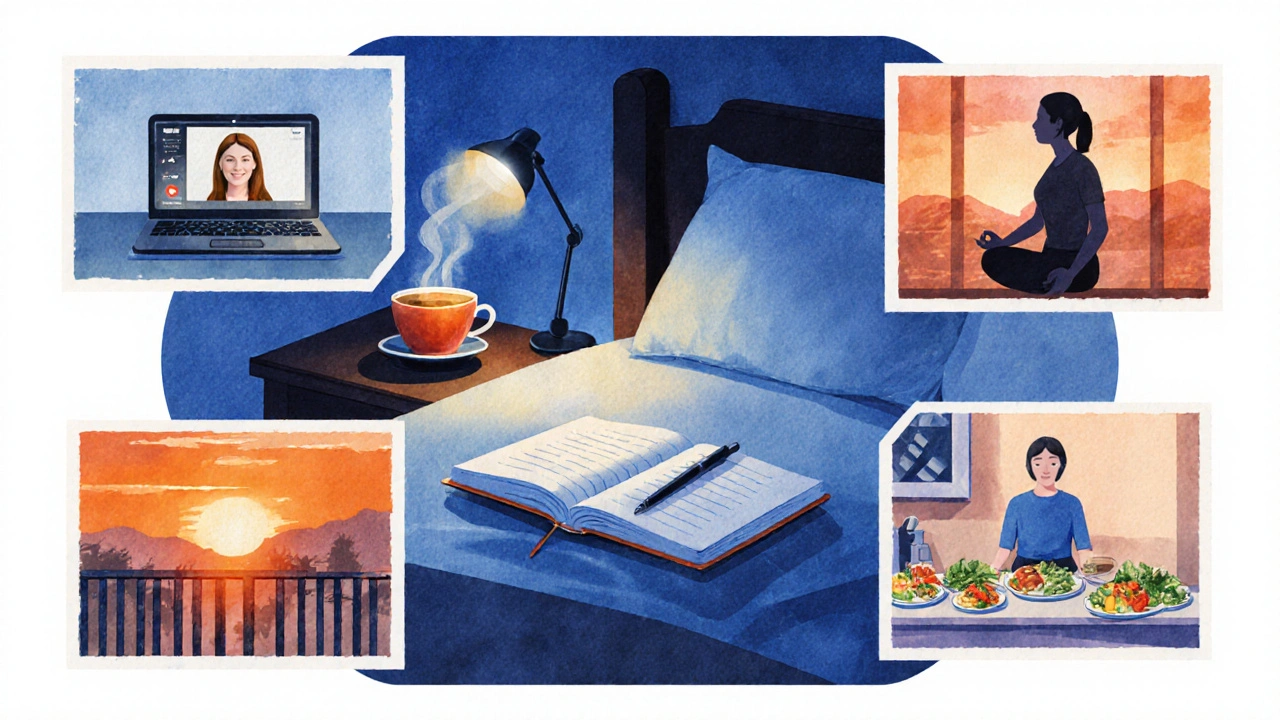
Integrating Therapy into Your Care Plan
Think of therapy as a fourth pillar alongside medication, diet, and exercise. Here’s a simple weekly rhythm:
- Monday - Review medication schedule with your gastroenterologist during a brief check‑in.
- Wednesday - Attend a 45‑minute CBT session (in‑person or virtual).
- Friday - Practice a 10‑minute mindfulness exercise before dinner.
- Sunday - Log symptoms, stress level, and diet in a journal; share highlights with your therapist if comfortable.
This routine creates feedback loops: therapist sees patterns, helps tweak coping tools, and you notice fewer flare triggers.
Quick Checklist for Starting Therapy
- Ask your gastroenterologist for a mental health referral.
- Confirm your health fund’s mental health care plan requirements.
- Choose a therapy type that matches your personality and symptom pattern.
- Schedule the first session and set a clear goal (e.g., “reduce flare frequency by 20%”).
- Track stress, sleep, and bowel symptoms weekly.
- Review progress with both therapist and doctor after 8 weeks.
Frequently Asked Questions
Can therapy actually prevent colitis flare‑ups?
Yes. By lowering stress hormones like cortisol, therapy reduces the inflammatory cascade that can trigger flares. Studies show a 30% decrease in severe flares for patients who receive regular CBT or mindfulness training.
Do I need a special kind of therapist for colitis?
A therapist with experience in chronic illness or IBD is ideal, but any licensed psychologist who uses evidence‑based techniques (CBT, MBSR) can be effective. Mention your diagnosis early, so they can tailor examples to gut‑related stress.
Is therapy covered by Australian health insurance?
Most private health funds reimburse a set number of sessions if you have a GP‑issued mental health care plan. Medicare also provides rebates for eligible mental health services under the Better Access Scheme.
How long does it take to see benefits?
Clients often notice reduced anxiety and better sleep within 4‑6 weeks. Improvements in flare frequency typically become evident after 8‑12 weeks of consistent therapy.
Can I combine therapy with other supportive practices?
Absolutely. Pairing CBT with a low‑FODMAP diet, regular low‑impact exercise, and probiotic guidance creates a holistic plan that addresses both mind and gut.

Heather Jackson
October 12, 2025 AT 04:17Therapy 4 colitis? Totally a game‑changer!
Akshay Pure
October 13, 2025 AT 08:04The notion that mere psychological support can substantively mitigate colitis flare‑ups is, in my estimation, a simplistic reduction of a profoundly intricate immunological cascade.
One must first acknowledge that the gut–brain axis, while undeniably influential, operates within a labyrinthine network of neuroendocrine feedback loops that defy reductionist therapeutic models.
To attribute a 30 % diminution in severe flares to routine counseling is an overstatement that betrays a lack of appreciation for the underlying mucosal pathology.
It is incumbent upon clinicians to prioritize evidence‑based pharmacological interventions before heralding psychotherapy as a panacea.
Nonetheless, the psychosocial dimensions of chronic disease cannot be dismissed as trivial footnotes.
Patients who internalize stigma or experience heightened anxiety may indeed experience secondary exacerbations of their inflammatory state.
In this respect, adjunctive mental health support serves as a valuable complement rather than the primary driver of remission.
The literature, while supportive of integrative care, consistently emphasizes a multimodal approach that balances biologic, dietary, and psychological strategies.
From a methodological standpoint, many studies suffer from limited sample sizes and heterogeneous outcome measures, casting doubt on the generalizability of the quoted 30 % figure.
Moreover, the placebo effect, especially in chronic pain and discomfort contexts, can inflate perceived benefits.
Thus, one should adopt a measured perspective, recognizing mental health therapy as an enhancer of overall well‑being rather than a solitary cure.
Clinicians must also ensure that patients are not diverted from essential medication adherence under the guise of 'therapy sufficiency.'
A collaborative care model, wherein gastroenterologists, dietitians, and psychologists co‑manage the patient, is arguably the gold standard.
In practice, such interdisciplinary teams have demonstrated modest but consistent improvements in quality‑of‑life indices.
Therefore, while mental health support is certainly advantageous, it should be contextualized within a broader, evidence‑grounded treatment paradigm.
Steven Macy
October 14, 2025 AT 11:50I hear the concerns about over‑promising mental health benefits, and it's a valid point. At the same time, the lived experience of anxiety during a flare can be overwhelming, and even a modest reduction in stress can translate into fewer triggers. From a holistic perspective, nurturing the mind and the gut offers a synergistic pathway toward stability. Ultimately, we should strive for a balanced regimen that respects both the body’s biology and the mind’s resilience.
Artie Alex
October 15, 2025 AT 15:37The preceding discourse aptly delineates the adjunctive role of psychotherapy within a polytherapeutic schema. Accordingly, clinicians ought to integrate psychotherapeutic modalities as a complementary vector rather than a monolithic solution.
abigail loterina
October 16, 2025 AT 19:24Great points, everyone. It’s amazing how a little counseling can lift mood and help you cope with the ups and downs of colitis. Keep sharing your stories and supporting each other!
Roger Cole
October 17, 2025 AT 23:10Therapy isn’t a cure‑all, but it sure helps.
Chris Wiseman
October 19, 2025 AT 02:57Picture this: a sailor navigating a stormy sea, his compass flickering between hope and dread-that's the daily trek of a colitis patient battling flare‑ups. When you sprinkle a dash of therapy into that turbulent mix, you’re essentially handing the sailor a sturdy telescope to glimpse calmer waters ahead. The mind, you see, is a rubber band that can stretch, snap, or rebound depending on the tension you apply. By engaging in consistent mental‑health practices, you’re not just loosening the knot of anxiety; you’re re‑weaving the very fabric of resilience. Think of cognitive‑behavioral techniques as the wind that fills the sails, propelling you forward even when the tide is low. A robust support network acts like a lighthouse, offering guidance when darkness threatens to engulf you. While no single approach guarantees salvation, the mosaic of therapy, diet, and medication forms a tapestry rich with possibilities. So, strap on that metaphorical life‑jacket, and let the currents of holistic care carry you toward steadier horizons.
alan garcia petra
October 20, 2025 AT 06:44Exactly, every little boost counts toward a brighter day!
Francisco Garcia
October 21, 2025 AT 10:30I’m curious about how different cultural attitudes toward mental health influence patient compliance. In some societies, seeking therapy carries a stigma that may deter people from accessing potentially beneficial support. Conversely, communities that normalize psychological care often report better disease management outcomes. It would be valuable to see comparative data across regions. Understanding these nuances could help tailor outreach programs effectively.
Patrick Renneker
October 22, 2025 AT 14:17While the foregoing observations possess a veneer of plausibility, one must critically appraise the epistemological foundations upon which they rest. The extant corpus of randomized controlled trials concerning psychotherapeutic interventions in colitis is, regrettably, scant and fraught with methodological heterogeneity. Consequently, any extrapolation of modest effect sizes to universal clinical practice remains speculative at best. A sober appraisal necessitates acknowledging the potential confounding variables, including socioeconomic status and concomitant comorbidities. Moreover, the proclivity for selection bias in observational cohorts cannot be dismissed without rigorous statistical remediation. Hence, prudence dictates that mental health support be integrated judiciously, pending more definitive empirical substantiation.
KAYLEE MCDONALD
October 23, 2025 AT 18:04Mental health care isn’t optional for chronic illness; it’s essential. Prioritize it alongside meds.
Alec McCoy
October 24, 2025 AT 21:50Let’s keep the momentum going-every session, every breathing exercise, every check‑in is a step toward reclaiming control. Remember, progress isn’t always linear, but persistence builds endurance. Share the wins, no matter how small, and lift each other up in the tough moments. Together, we can transform the narrative from suffering to thriving.