Epidural Hematoma: Causes, Symptoms, and What You Need to Know
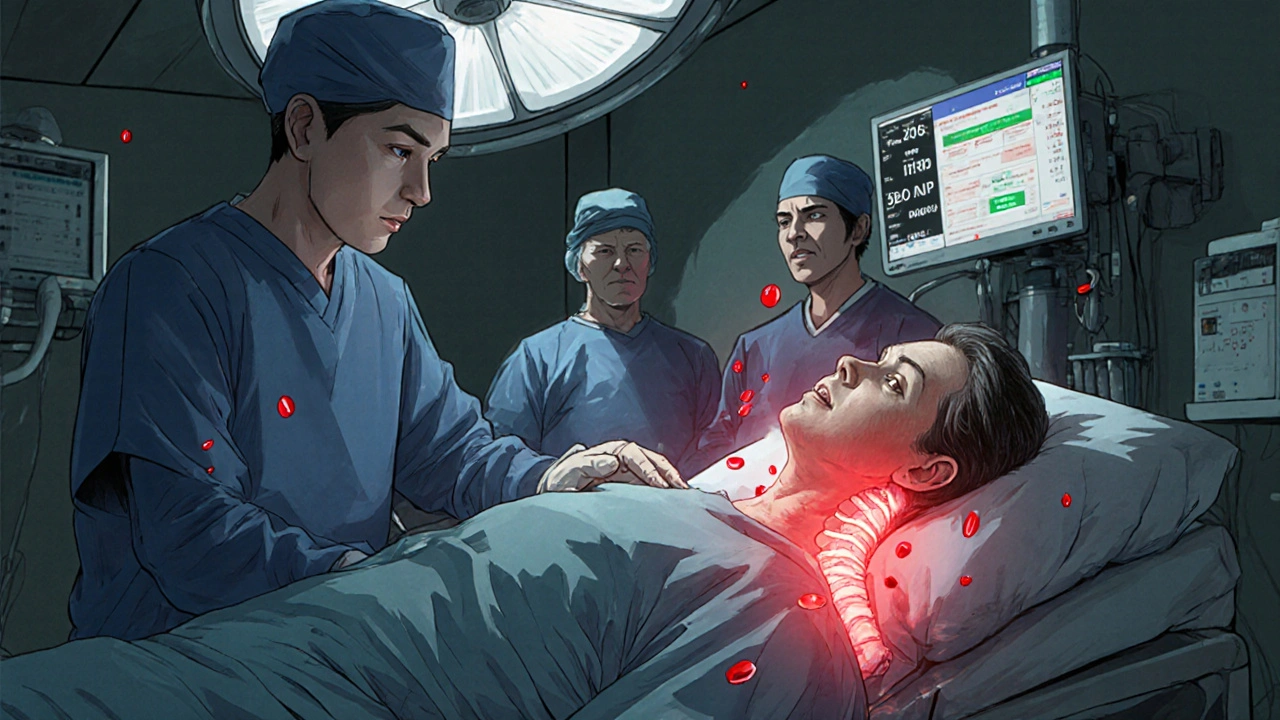
When you hit your head hard enough, something dangerous can happen inside your skull: an epidural hematoma, a collection of blood between the skull and the dura mater, the brain’s tough outer membrane. Also known as extradural hematoma, it’s not a slow-developing issue—it’s a medical emergency that can kill within hours if ignored. This isn’t just a bruise. It’s bleeding that builds pressure on the brain, squeezing vital tissue and cutting off oxygen.
This type of bleeding usually follows a sharp blow to the head, like a fall, car crash, or sports injury. The most common cause? A fracture in the temporal bone, which tears the middle meningeal artery. That’s the blood vessel right under the side of your skull. Once it bleeds, blood pools fast—sometimes in under 15 minutes. You might feel fine at first, then suddenly get worse. That’s the classic pattern: lose consciousness briefly, wake up alert, then start having a headache, confusion, or vomiting. It’s called the "lucid interval," and it’s dangerously misleading.
Doctors diagnose it with a CT scan, which shows the blood as a bright, lens-shaped area. Time is everything. If caught early, a neurosurgeon can drill a hole in the skull to drain the blood—simple, fast, and life-saving. Delay it, and the pressure can push the brain down, stop breathing, or trigger a stroke. Even with treatment, some people have lasting problems like memory loss or trouble concentrating. That’s why anyone who takes a hard hit to the head needs to be watched closely for at least 24 hours, even if they seem okay.
Children and young adults are most at risk because their skulls are thinner and their blood vessels more fragile. But it can happen to anyone. If you or someone you know has had a head injury and then starts acting strange—slurred speech, weakness on one side, seizures, or extreme drowsiness—don’t wait. Call 911. No home remedy, ice pack, or "just rest" will fix this.
What you’ll find below are real, practical posts that connect directly to this condition. You’ll read about how head trauma leads to complications, how medications are managed during recovery, and how other brain-related injuries compare. These aren’t abstract theories. They’re insights from people who’ve lived through this, or doctors who treat it daily. Whether you’re worried after an accident, supporting someone in recovery, or just trying to understand what really happens inside the skull after trauma—this collection gives you the facts you need, without the fluff.