Biosimilar vs Generic: What’s the Real Difference?
When you hear generic drugs, lower-cost versions of brand-name medicines that contain the same active ingredient and work the same way in the body. Also known as non-branded drugs, they’re the go-to for saving money on pills like metformin or lisinopril. But if your doctor mentions a biosimilar, a highly similar version of a complex biologic drug made from living cells, not chemicals. Also known as biologic copycats, it’s a whole different story. Generics are chemical copies. Biosimilars are biological copies—and that changes everything.
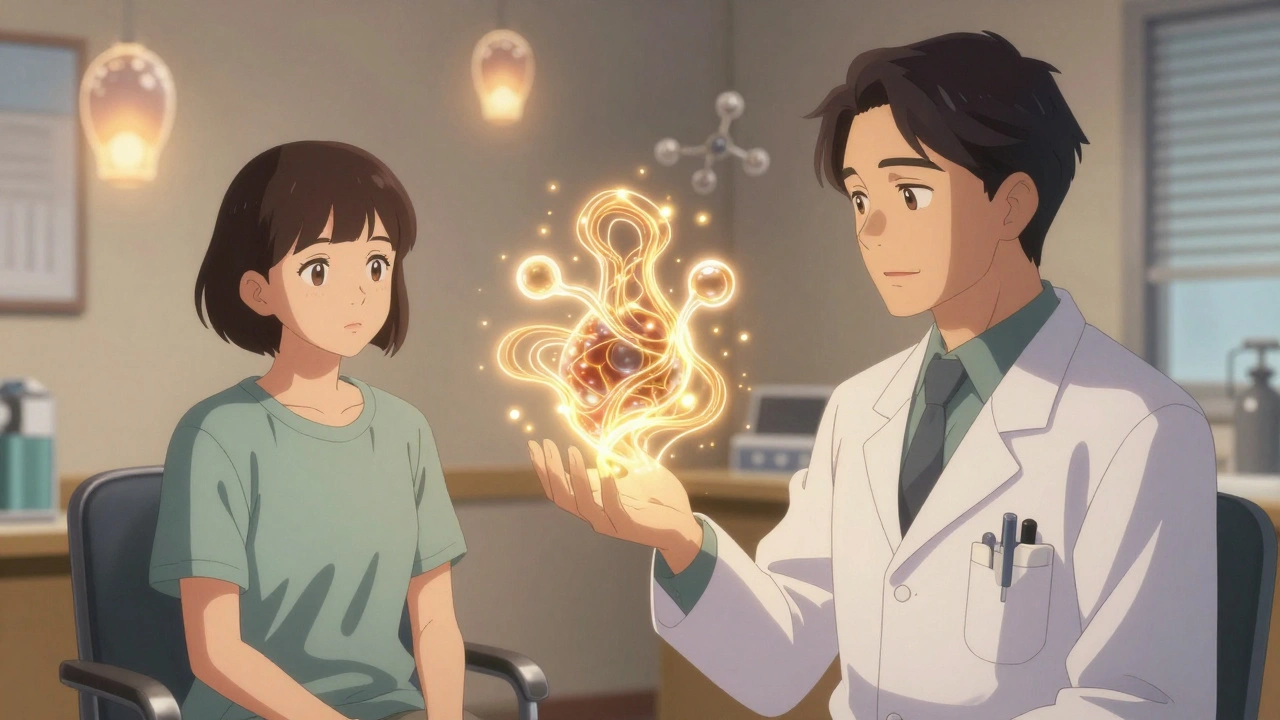
Think of it like this: a generic drug is like copying a simple recipe—same flour, sugar, eggs. You get the same cake. A biosimilar, a version of a biologic drug that’s made using living organisms like bacteria or yeast, making it far more complex than a chemical compound is like trying to copy a sourdough starter. Even with the same ingredients, the microbes, temperature, and time make every batch slightly different. That’s why biosimilars can’t be called "identical"—they’re "highly similar" with no clinically meaningful differences in safety or effectiveness. The FDA requires way more testing for biosimilars than generics. While generics just need to prove they absorb the same way in your blood (pharmacokinetic studies), biosimilars need full clinical trials showing they work the same in real patients—often for conditions like rheumatoid arthritis, cancer, or diabetes.
That’s why you won’t find a biosimilar for aspirin. Biosimilars only exist for biologic drugs, medications made from living sources, like antibodies or proteins, used to treat complex chronic diseases—think Humira, Enbrel, or Rituxan. Generics? They’re for the simple stuff: antibiotics, blood pressure pills, antidepressants. And here’s the kicker: even though biosimilars are cheaper than the original biologic, they’re still way more expensive than generics. That’s because making a living cell-based drug is like brewing craft beer in a lab—it’s finicky, expensive, and hard to scale.
So why does this matter to you? If you’re switching from a brand-name biologic to a biosimilar, your doctor should explain why it’s safe. You won’t get a generic version of a biologic—it’s not possible. But you might get a biosimilar, and it’s often covered by insurance with lower co-pays. If you’re on a generic pill, you can usually swap brands without a second thought. But if you’re on a biologic, don’t assume the biosimilar is just another generic. The science, the testing, and the risks are different. That’s why you’ll find posts here about how pharmacists explain these differences to patients, how excipients in generics can cause reactions, and why pharmacokinetic studies are the gold standard for proving equivalence. You’ll also see how combo generics save money, how counterfeit pills mess with trust, and how to spot when a drug isn’t working like it should. This isn’t just about labels—it’s about your health, your safety, and knowing exactly what’s in your medicine.