Using steroid eye drops can be a game-changer for sudden eye inflammation - but only if you know how to use them safely. These drops, like prednisolone acetate, dexamethasone, and loteprednol etabonate, work fast to calm down redness, swelling, and pain from conditions like uveitis, allergic conjunctivitis, or eye burns. But they’re not harmless. Left unchecked, they can quietly damage your vision - sometimes before you even notice anything’s wrong.
Why Doctors Prescribe Steroid Eye Drops
Steroid eye drops don’t cure infections. They don’t kill bacteria or viruses. What they do is shut down inflammation. That’s critical when your eye is swollen from an autoimmune flare-up, an injury, or a severe allergic reaction. In cases of acute anterior uveitis, where the front part of the eye becomes inflamed, steroids can prevent permanent scarring that might blur your vision forever.
For many patients, the relief is immediate. Redness fades within a day or two. Pain drops off quickly. That’s why doctors reach for them when time matters. The goal isn’t to use them long-term - it’s to get the inflammation under control fast, then taper off. Most patients use them for one to two months, and that’s usually enough to heal without triggering major side effects.
The Hidden Dangers: Glaucoma and Cataracts
Here’s the catch: your eye doesn’t feel the damage until it’s too late.
One of the biggest risks is steroid-induced glaucoma. Steroids can cause pressure inside your eye - called intraocular pressure (IOP) - to spike. In 30-40% of people, there’s a mild rise. For 4-6%, it shoots up dangerously high. These people are called “steroid responders.” If you have a family history of glaucoma, diabetes, or already have high eye pressure, your risk is even higher.
The scary part? Glaucoma from steroids often has no symptoms. No pain. No redness. Just slowly losing your side vision. By the time you notice blurry spots or tunnel vision, the optic nerve may already be damaged - and that damage is permanent.
The second major threat is cataracts. Prolonged use - especially beyond 10 days - increases your chance of developing posterior subcapsular cataracts. These form at the back of the lens, right in the center of your vision. They make light scatter, causing glare, halos, and blurry vision, especially at night. Unlike age-related cataracts, these can develop in just a few months of steroid use. Studies show they can bring forward the need for cataract surgery by 5 to 10 years.
Infection Risk: When Steroids Backfire
Steroids suppress your eye’s natural defenses. That’s great for calming inflammation - but terrible if you have a hidden infection.
If you have a mild herpes simplex virus in your eye and start steroid drops, the virus can explode. Same with fungal infections. These can turn into corneal ulcers - painful, sight-threatening emergencies. That’s why doctors always check for infection before prescribing steroids. If your eye is red and irritated but you haven’t been diagnosed, don’t start steroid drops without seeing a specialist.
Even if you’ve used them safely before, don’t assume you’re immune. Your immune response changes over time. A drop that was fine last year could trigger an infection this year.
Who Needs Extra Monitoring?
Not everyone needs the same level of care. But some people need more frequent checks:
- People with pre-existing glaucoma
- Those with diabetes
- Anyone with a family history of glaucoma or cataracts
- Patients using high-potency drops like prednisolone acetate
- Anyone on steroids for more than two weeks
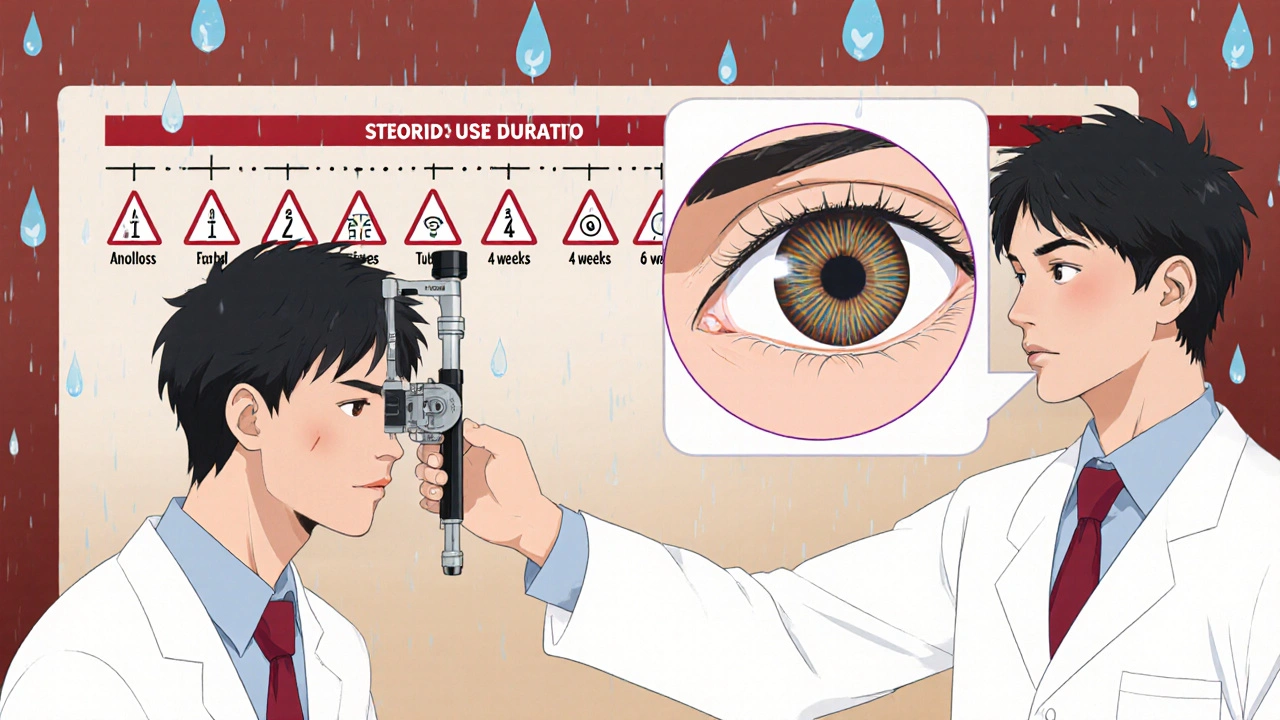
If you fall into any of these groups, your eye doctor should check your eye pressure every 1-2 weeks during treatment. For others, every 2-4 weeks is standard. Baseline pressure should be measured before you even start the drops.
Regular exams aren’t optional. They’re your safety net. Your doctor will use a tool called a Goldmann applanation tonometer to measure pressure accurately. They’ll also look at your optic nerve and lens with a slit lamp - a high-powered microscope that reveals early signs of damage you can’t feel.
How Long Is Too Long?
There’s no universal safe time. But there are clear danger zones:
- Less than two weeks: Low risk for most people, especially with low-dose drops.
- Two to four weeks: Moderate risk. Watch for symptoms.
- More than four weeks: High risk. Glaucoma and cataract chances rise sharply.
- Three to six months: Very high risk. Cataract development becomes likely.
Most uveitis patients get better in 4-8 weeks. If you’re still on drops after that, your doctor should be reevaluating your treatment. Maybe you need a different drug. Maybe you need a lower dose. Or maybe you need to switch to a non-steroidal option.
Alternatives to Steroids
For chronic conditions - like recurring allergies or autoimmune uveitis - doctors are turning more often to non-steroidal anti-inflammatory drugs (NSAIDs) for the eye. These don’t have the same power as steroids, but they also don’t raise eye pressure or cause cataracts.
Some patients use them alone. Others use them after tapering off steroids to keep inflammation down without the risks. If your condition flares up often, talk to your eye doctor about whether NSAIDs could be part of your long-term plan.
What Symptoms Should Worry You?
Even if you’re being monitored, pay attention to your own eyes. Call your doctor right away if you notice:
- Blurry vision that doesn’t improve
- Eye pain or pressure
- Seeing halos around lights
- Loss of side vision
- Redness returning after it had cleared
- Nausea or headaches with eye pain
These aren’t normal side effects. They’re warning signs. Don’t wait for your next appointment.
Never Stop Suddenly
Stopping steroid drops cold turkey can cause your inflammation to come back worse than before - a rebound effect. Your doctor will give you a tapering schedule. Maybe you go from four times a day to twice a day, then every other day, then stop. Follow it exactly.
If you miss a dose, don’t double up. Just go back to your regular schedule. If you run out, call your doctor before refilling. Don’t use old drops without checking if they’re still safe.
What Happens If You Need Cataract Surgery?
If steroid use leads to cataracts, surgery is usually the only fix. It’s one of the most common and successful surgeries in the world - about 95% of patients regain clear vision. But it’s still surgery. There’s a small risk of infection (less than 0.1%) or a cloudy membrane forming behind the new lens (called posterior capsule opacification), which happens in about 20% of cases within five years. That’s easily fixed with a quick laser procedure.
But the best outcome? Never needing surgery at all. That’s why monitoring matters more than anything.
Final Advice: Use Smart, Not Just When It Hurts
Steroid eye drops are powerful tools. They’ve saved sight for millions. But they’re not candy. They’re more like a scalpel - useful in skilled hands, dangerous if misused.
If your doctor prescribes them, ask: How long? How often? What signs should I watch for? When will we check my pressure again?
And if you’ve been using them for more than two weeks without a follow-up - get one. Your vision doesn’t have a backup plan. But you do.
Can steroid eye drops cause blindness?
Yes, if used improperly or without monitoring. Long-term use can lead to steroid-induced glaucoma, which damages the optic nerve, or cataracts that severely blur vision. Both can cause permanent vision loss if not caught early. Most cases are preventable with regular eye pressure checks and timely discontinuation.
How often should eye pressure be checked while using steroid drops?
For most people, every 2-4 weeks. For high-risk patients - those with glaucoma, diabetes, or a family history - check every 1-2 weeks. Baseline pressure should be measured before starting treatment. More frequent checks are needed if you’re using high-potency drops like prednisolone acetate or using them longer than two weeks.
Are there steroid eye drops that are safer than others?
Yes. Loteprednol etabonate is considered a lower-risk steroid because it breaks down quickly in the eye, reducing the chance of pressure buildup. Prednisolone acetate is stronger and carries higher risk. Your doctor chooses based on your condition and risk profile. Even “safer” steroids need monitoring if used beyond two weeks.
Can I use steroid eye drops for red eyes from contacts?
No - not without seeing a doctor first. Red eyes from contacts are often due to infection, irritation, or lack of oxygen. Steroid drops can mask infection and make it worse. Never use them for red eyes unless a professional confirms it’s non-infectious inflammation. Self-treating can lead to serious damage.
How long do steroid eye drops stay in your system?
They don’t stay in your bloodstream long - they’re designed to act locally in the eye. But their effects on eye pressure and lens clarity can last weeks after you stop using them. That’s why monitoring continues even after you finish the prescription. The damage they cause, if any, can be permanent.
Can children use steroid eye drops?
Yes, but with extreme caution. Children are more sensitive to steroid side effects, including pressure spikes and cataract formation. They require close monitoring by a pediatric ophthalmologist. Use is typically limited to short courses for severe inflammation, and doses are carefully adjusted by weight and age.
What happens if I forget to go to my follow-up appointment?
You’re putting your vision at risk. Eye pressure can rise without symptoms, and cataracts develop slowly. Missing one check-up might mean missing the early warning signs. If you miss an appointment, reschedule immediately. Don’t wait until you notice a problem - by then, it may be too late.
Are there natural alternatives to steroid eye drops?
There are no proven natural alternatives that match the strength of steroids for severe inflammation. However, for mild allergies, cold compresses, artificial tears, and antihistamine drops can help. For chronic conditions, non-steroidal anti-inflammatory eye drops (NSAIDs) are the closest medical alternative. Never replace steroids with herbs or home remedies without medical advice - it could delay treatment and worsen damage.

Kihya Beitz
November 14, 2025 AT 08:18So let me get this straight - we’re giving people chemical scalpels to poke their own eyes and calling it ‘medicine’? And the only safety net is ‘oh, just check your pressure every few weeks’? Lol. My grandma’s cat has more consistent monitoring than this. I’ve seen people go blind from these drops because their doctor was ‘too busy’ to call back. This isn’t treatment - it’s Russian roulette with a cornea.
Jennifer Walton
November 15, 2025 AT 03:41Controlled inflammation is not healing. It’s suppression. The body doesn’t heal by quieting signals - it heals by resolving the cause. Steroids are a linguistic trick: they make pain disappear so we forget to ask why it was there in the first place.
Shyamal Spadoni
November 16, 2025 AT 10:18yo i read this whole thing and im like bro what if the FDA is just letting big pharma push these drops so people end up needing cataract surgery and then they gotta buy new lenses and then the hospitals make bank?? i mean look at the stats - 30-40% get pressure spikes?? thats not coincidence thats a business model. and dont even get me started on how they say ‘dont stop suddenly’ - thats just to keep you hooked like a drug addict. i think they put steroids in the drops on purpose so you get addicted to the relief and then boom - you need surgery. also i heard the tonometer is fake and they just guess the pressure. my cousin in delhi says the machines are programmed to show normal even when its sky high. this is all a scam. i’m not taking these drops. i’m using turmeric and cold tea bags now. its working better than my doctor said it would.
Ogonna Igbo
November 16, 2025 AT 12:03Listen here this is why Africa and India are ahead in natural medicine. You westerners always reach for chemicals first. In Nigeria we use honey and neem oil for eye inflammation. It’s been done for centuries. Your doctors are just scared of losing money. Steroid drops? That’s colonial medicine. We don’t need your expensive machines and your ‘Goldmann’ nonsense. My uncle had uveitis and used crushed papaya leaf paste - healed in 10 days. No pressure checks. No cataracts. Just real medicine. Why are you letting corporations poison your eyes when nature already gave you the cure?
BABA SABKA
November 18, 2025 AT 00:13Let’s cut through the noise. The real issue here isn’t the drops - it’s the systemic failure of ophthalmology to prioritize monitoring. You’ve got a $5000 tonometer sitting in a clinic that sees 50 patients a day and a nurse who’s never been trained to interpret the readings. The ‘safe’ protocols are theoretical. Real-world execution? Garbage. I’m a med tech. I’ve seen it. Patients get prescribed 4 weeks of prednisolone acetate and then vanish. No follow-up. No pressure logs. No slit-lamp checks. And then they show up six months later with glaucoma and blame the ‘drug’. No. They blamed the system. And the system didn’t care enough to stop them. This isn’t a drug problem. It’s a healthcare infrastructure collapse dressed up as a patient education piece.
Chris Bryan
November 19, 2025 AT 01:34Of course they’re pushing this. It’s all part of the Great Eye Deception. The WHO, the AMA, the FDA - all in bed with the big pharma cabal. They want you dependent. They want you coming back every month. They want you scared of your own vision. They know if you used NSAIDs or natural remedies, you’d save money and they’d lose billions. And that’s why they lie about ‘steroid responders’ - it’s a cover to justify endless monitoring fees. Don’t fall for it. I stopped all drops after reading this. Used raw garlic compresses. Vision improved. No more halos. No more pressure. The system hates truth.
Jonathan Dobey
November 19, 2025 AT 07:42Ah, the tragic ballet of modern medicine: we weaponize the body’s own language of pain - silence it with synthetic silence - and then wonder why the patient wakes up blind. Steroid eye drops are not treatment; they’re a poetic erasure. A temporary ceasefire in a war the body never agreed to fight. We’ve turned the eye - that cathedral of perception - into a chemical test tube. And the doctors? They’re not healers. They’re conductors of a slow-motion symphony of iatrogenic ruin. You don’t need more monitoring. You need to stop playing God with your cornea. Let inflammation burn. Let it teach. Let the eye remember how to heal itself - even if it takes longer. Because what is vision, if not the soul’s ability to witness truth? And what is a steroid, if not a lie dressed in sterile packaging?
ASHISH TURAN
November 20, 2025 AT 18:27My dad used steroid drops for uveitis back in 2015. He followed every check-up, had his pressure taken every 10 days, and tapered slowly. No cataracts. No glaucoma. It’s not the drops that are dangerous - it’s the neglect. If you treat them like candy, they’ll bite you. Treat them like a tool - with respect, structure, and follow-up - and they can save your sight. Don’t blame the medicine. Blame the silence between appointments. The system works if you show up.