Drug Rash Risk Assessment Tool
Assess Your Risk
This tool helps you identify potential medication-induced skin reactions based on your symptoms and medications. It is not a substitute for professional medical advice.
More than 1 in 20 people taking prescription or over-the-counter medications will develop a skin rash because of it. It’s not always an allergy. It’s not always serious. But it can be. And if you don’t know the difference, you could miss the warning signs of something life-threatening.
What Does a Drug Rash Look Like?
Drug rashes come in many shapes and sizes. The most common type - called a morbilliform or maculopapular rash - looks like small red bumps or flat spots that spread symmetrically across your chest, back, and upper arms. It usually shows up 4 to 14 days after you start a new medicine. You might feel a little warm or itchy, but you won’t feel like you’re dying. This rash accounts for 90% of all drug-induced skin reactions and almost always goes away on its own once you stop the medication.
Then there’s the less common but far more dangerous kind. Think blistering skin, peeling like a sunburn, or large, painful red patches. These are signs of severe cutaneous adverse reactions (SCARs) like Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). These are medical emergencies. Between 5% and 15% of people who develop SJS don’t survive. TEN has an even higher death rate - up to 35%. If you notice blisters forming in your mouth, eyes, or genitals, or if large areas of skin are peeling off, go to the emergency room right now.
Another type you might mistake for eczema is nummular dermatitis. It shows up as coin-shaped, red, scaly patches, often on the legs or arms. It can be caused by antibiotics, blood pressure meds, or even supplements. Doctors often misdiagnose this as regular eczema - up to 40% of the time. The difference? A drug-induced version clears up in 4 to 8 weeks after stopping the medicine. Regular eczema can last years.
Which Medications Cause Rashes?
Not all drugs are equal when it comes to triggering skin reactions. Some are far more likely to cause trouble.
- Antibiotics - especially penicillin and sulfa drugs - are responsible for nearly half of all allergic drug rashes. Penicillin alone causes 80% of severe allergic reactions to medications.
- Antiseizure medicines like carbamazepine, phenytoin, and lamotrigine can trigger DRESS syndrome - a delayed reaction that affects your skin, liver, kidneys, and blood. It shows up weeks after starting the drug and comes with fever, swollen glands, and high white blood cell counts.
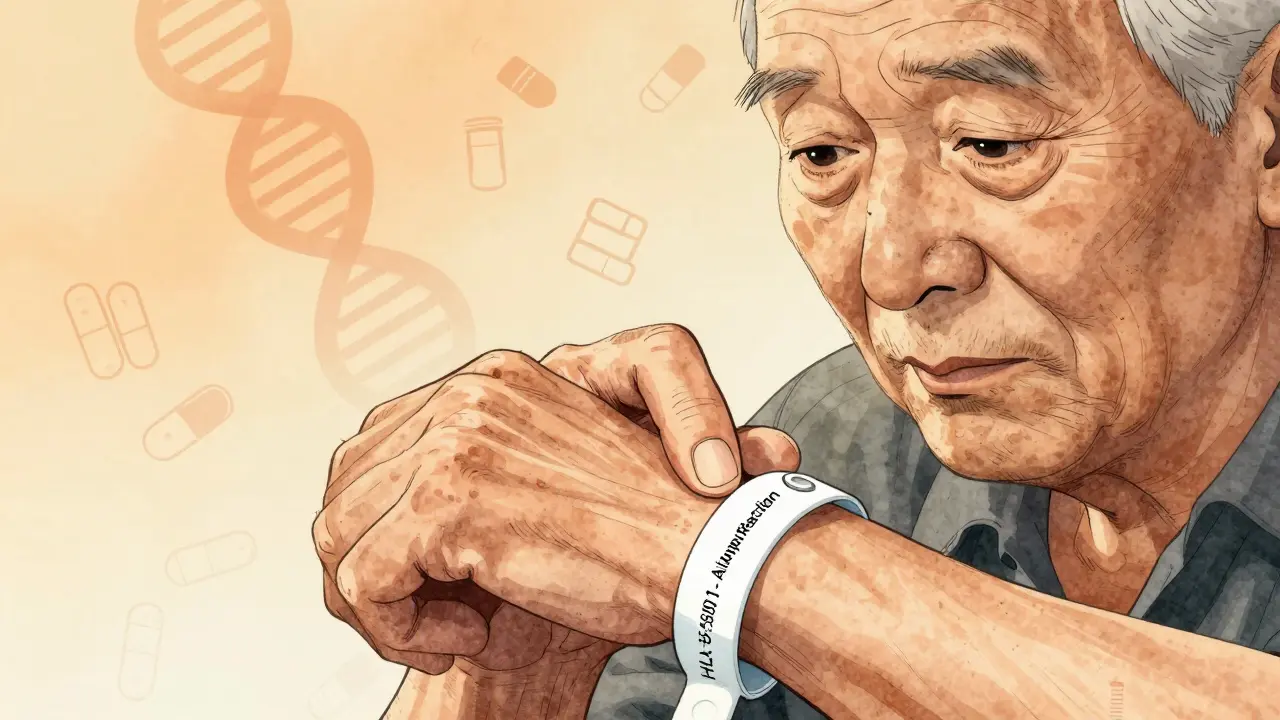
- Allopurinol (used for gout) is a major culprit in SCARs, especially in people of Asian descent with a specific gene variant (HLA-B*5801).
- NSAIDs like ibuprofen and naproxen don’t always cause true allergies. Instead, they trigger non-allergic reactions that mimic hives or swelling - especially in people with asthma or nasal polyps.
- Chemotherapy drugs and antivirals are also common triggers, especially in people with weakened immune systems.
- Topical meds - like neomycin in antibiotic creams or poison ivy lotions - can cause contact dermatitis. These are localized, not full-body.
And here’s something most people don’t realize: you don’t need to be allergic the first time you take a drug. Your immune system can learn to react after a single exposure. That’s why someone might take amoxicillin five times without issue - then break out in a rash on the sixth. It’s not a mistake. It’s biology.
How to Tell If It’s Allergic or Not
Not every rash from a drug is an allergy. In fact, most aren’t.
Allergic reactions involve your immune system. They usually take days to appear. They can get worse with repeated exposure. They often come with itching, hives, swelling, or breathing trouble. Penicillin allergies fall into this category.
Non-allergic reactions are direct toxic effects. Your body doesn’t make antibodies - it just reacts badly to the chemical. These can happen the first time you take the drug. Think of aspirin causing hives in someone with asthma, or morphine triggering flushing and itching. These aren’t allergies, but they still need to be treated seriously.
The timing tells you a lot. If the rash shows up within an hour of taking the pill, it’s likely an IgE-mediated allergy - think hives or anaphylaxis. If it shows up after a week or two, it’s probably a T-cell reaction - the kind linked to DRESS or SJS. This distinction matters because it changes how you treat it and what you avoid in the future.

What to Do If You Get a Rash
Here’s the rule: never stop a prescribed medication on your own. Especially if it’s for epilepsy, heart disease, or mental health. Stopping suddenly could kill you faster than the rash.
Instead, call your doctor. Take a photo of the rash. Note when you started the medication and when the rash appeared. List every drug you’re taking - even vitamins and herbal supplements. Many rashes are caused by interactions, not single drugs.
If it’s mild - just red bumps, no blisters, no trouble breathing - your doctor might tell you to keep taking the drug and use over-the-counter hydrocortisone cream twice a day. Lukewarm baths with fragrance-free cleansers and moisturizer applied within 3 minutes of drying can help soothe the skin.
If it’s severe - blisters, peeling, fever, swelling in your face or throat - go to the ER. Don’t wait. Don’t call your doctor first. Go. These reactions can turn deadly in hours.
And if you’ve had a serious reaction before, wear a medical alert bracelet. List the drug and the reaction. It could save your life if you’re ever unconscious in an emergency.
Who’s at Higher Risk?
Some people are far more likely to develop drug rashes.
- People over 65 - they take more medications. Someone on five or more drugs has a 35% chance of developing a drug rash in their lifetime. That’s 7 times higher than someone on just one or two.
- People with HIV or Epstein-Barr virus - if you’re taking antibiotics while fighting a viral infection, your risk of a severe rash jumps 5 to 10 times.
- People with autoimmune diseases or cancer - weakened immune systems mean your body reacts more unpredictably to drugs.
- People of Southeast Asian or Han Chinese descent - if you carry the HLA-B*1502 or HLA-B*5801 gene variants, you’re at extreme risk for SJS or DRESS from certain drugs. Genetic testing before prescribing carbamazepine or allopurinol is now standard in many countries.
- People with a history of drug rashes - once you’ve had one, your chances of having another go up.
And here’s a hidden risk: photosensitivity. Some drugs make your skin super sensitive to sunlight. Doxycycline, hydrochlorothiazide, and ciprofloxacin are big ones. You might think you’re just sunburned - but it’s actually a drug reaction. Wear sunscreen, cover up, and ask your pharmacist if any of your meds increase sun sensitivity.
Testing and Diagnosis
There’s no single test that confirms every drug rash. But some tools help.
For penicillin, skin testing is 95% accurate. If you think you’re allergic, get tested. About 15% of people who say they’re allergic to penicillin aren’t - they just had a rash years ago. Avoiding penicillin unnecessarily means you get stronger, more expensive antibiotics that carry higher risks of side effects and antibiotic resistance.
For DRESS or SJS, doctors look at blood tests: high eosinophils, abnormal liver enzymes, elevated creatinine. A skin biopsy can confirm the type of reaction. It’s not always needed for mild rashes, but it’s critical when the reaction is severe.
Genetic testing is becoming more common. If you’re about to start carbamazepine and you’re from Southeast Asia, your doctor should check for HLA-B*1502. If you’re about to take allopurinol and you’re Han Chinese, they should check for HLA-B*5801. These tests can prevent life-threatening reactions before they start.
What Happens After the Rash?
Most mild rashes clear up in 1 to 2 weeks after stopping the drug. You might feel itchy for a few days, but the skin returns to normal.
Severe reactions like DRESS take longer - often 3 to 6 weeks of steroid treatment. Some people need hospital care. Recovery can take months. And once you’ve had a severe reaction, you’re at higher risk for future ones - even with different drugs.
You’ll need to avoid the offending drug forever. And often, you’ll need to avoid other drugs in the same class. If you had a reaction to amoxicillin, you’ll likely need to avoid all penicillins. If you reacted to carbamazepine, you may need to avoid other antiseizure drugs like phenytoin or oxcarbazepine.
Keep a list of all drugs that caused reactions - and why. Share it with every new doctor. Even if you think it’s old news. It’s not.
Prevention Is Possible
You can’t always prevent a drug rash - but you can reduce your risk.
- Only take medications you truly need. Avoid unnecessary antibiotics or NSAIDs.
- Tell every doctor you see about every drug you’ve ever reacted to - even if it was years ago.
- Ask if your medication has a known risk for skin reactions - especially if you’re over 65 or have a chronic illness.
- Ask about genetic testing if you’re starting high-risk drugs like carbamazepine or allopurinol.
- Use one pharmacy for all your prescriptions. They can flag dangerous interactions.
- Don’t ignore a new rash. Even if it seems small.
Medications save lives. But they can also hurt you - silently, slowly, and sometimes fatally. The key isn’t avoiding medicine. It’s knowing how to recognize the warning signs - and acting fast.
Can a drug rash happen the first time you take a medication?
Yes. While some drug rashes only appear after repeated exposure, others - especially non-allergic reactions - can happen the very first time you take the medicine. This is common with NSAIDs like ibuprofen or antibiotics in people with viral infections. Your body doesn’t need to be "sensitized" first to react badly.
How long does a drug rash last after stopping the medicine?
Mild rashes usually fade within 1 to 2 weeks after stopping the drug. More severe reactions like DRESS or AGEP can take weeks to months to fully resolve, even after the drug is out of your system. Skin peeling from SJS/TEN may take months to heal completely.
Can I take the same drug again if the rash went away?
Never. Even if the rash was mild and went away on its own, your immune system remembers. Taking the same drug again - even years later - can trigger a much worse reaction, including life-threatening conditions like SJS or anaphylaxis. Avoid the drug completely and tell all future doctors.
Are over-the-counter creams safe for drug rashes?
For mild rashes, hydrocortisone 1% cream applied twice daily is generally safe and helpful. Avoid strong steroids like clobetasol unless prescribed. Never use antihistamine creams - they can irritate the skin more. Always check with your doctor first, especially if you have blisters or open skin.
Is a drug rash the same as an allergy?
No. A drug rash can be allergic (immune system involved) or non-allergic (direct chemical reaction). Most rashes are non-allergic. True drug allergies involve IgE antibodies and often cause hives, swelling, or breathing trouble. But you don’t need an allergy to get a serious rash - your body can react badly without immune involvement.
Should I get tested for drug allergies?
If you’ve had a severe reaction - especially to penicillin, sulfa, or antiseizure drugs - yes. Skin testing for penicillin is 95% accurate and can confirm whether you’re truly allergic. Many people who think they’re allergic aren’t. Getting tested can open up safer, cheaper treatment options.
Can I prevent drug rashes before they happen?
You can reduce your risk. Avoid unnecessary medications. Tell every doctor about past rashes. Ask about genetic testing if you’re starting high-risk drugs like carbamazepine or allopurinol - especially if you’re of Southeast Asian or Han Chinese descent. Use one pharmacy so your records are centralized. And never ignore a new rash - even if it seems minor.
Final Thoughts
Drug rashes are common. Most are harmless. But some are silent killers. The difference between life and death often comes down to one thing: knowing when to act. Don’t wait for a rash to get worse. Don’t assume it’s just dry skin. Don’t stop your meds without talking to your doctor. But do pay attention. Your skin is talking. Listen.

Brendan F. Cochran
January 4, 2026 AT 15:05jigisha Patel
January 6, 2026 AT 01:26Ethan Purser
January 6, 2026 AT 05:19Doreen Pachificus
January 6, 2026 AT 07:54Cassie Tynan
January 6, 2026 AT 08:43Rory Corrigan
January 7, 2026 AT 21:31Connor Hale
January 9, 2026 AT 08:45Charlotte N
January 9, 2026 AT 16:31Catherine HARDY
January 10, 2026 AT 01:55melissa cucic
January 10, 2026 AT 02:12