When you take a blood thinner like apixaban, rivaroxaban, or warfarin, you’re doing it to prevent a stroke or clot - not to risk bleeding to death. But the line between protection and danger is thin. Every year, tens of thousands of people on these medications end up in the emergency room because of uncontrolled bleeding. And too often, they wait too long to act.
Why Blood Thinners Cause Severe Bleeding
Blood thinners don’t actually make your blood thinner. They slow down the clotting process. That’s the whole point - to stop clots from forming in your heart, legs, or brain. But if you cut yourself, sneeze too hard, or fall, your body can’t seal the wound fast enough. The result? Bleeding that won’t stop. The most common culprits are anticoagulants like warfarin and the newer DOACs (direct oral anticoagulants): dabigatran, rivaroxaban, apixaban, and edoxaban. Antiplatelet drugs like clopidogrel also raise the risk. The American Heart Association found that over 28 months, people on clopidogrel had a 0.8% higher chance of moderate or severe bleeding than those not taking it. That might sound small, but when you’re the one bleeding, it’s life-changing. The risk isn’t random. It spikes in the first 90 days. One study showed that 60.8% of major bleeding events happened within the first three months of starting the medication. That’s when your body is still adjusting, and your doctor hasn’t yet figured out the right dose for you. Older adults, people with kidney problems, or those taking more than one blood thinner are at even higher risk.What Counts as a Severe Bleeding Episode
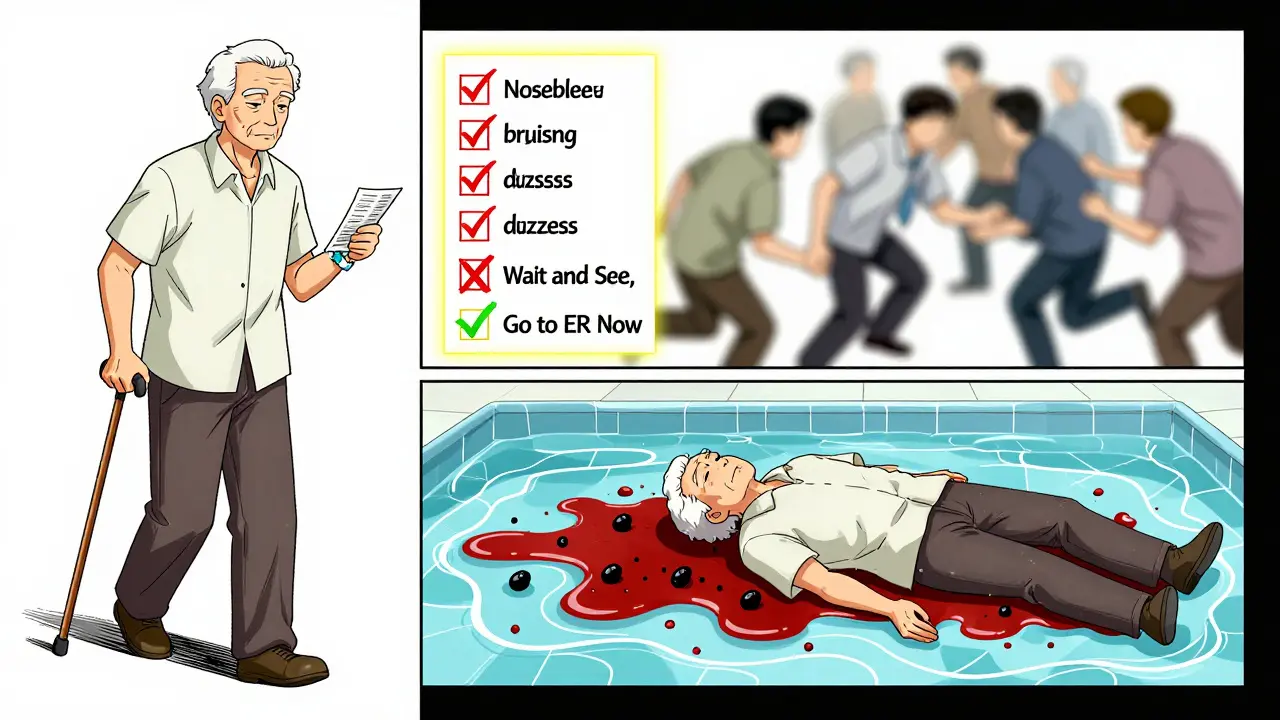
Not every nosebleed or bruise is an emergency. But some signs mean you need help right now:- Black, tarry stools - a sign of bleeding in your stomach or intestines
- Bloody or red-brown urine
- Vomiting blood or coughing up blood
- Unexplained, large bruises that keep growing
- Nosebleeds that last longer than 10 minutes
- Severe headache, dizziness, confusion, or vision changes - possible signs of bleeding in the brain
- Joint pain or swelling after a minor injury
- Excessive menstrual bleeding - more than soaking through a pad or tampon every hour
- Bleeding from a minor cut that won’t stop after 15 minutes of pressure
Who’s Most at Risk
Risk isn’t the same for everyone. Some factors make bleeding far more likely:- Age over 75: People over 80 have more than three times the bleeding risk of those under 60.
- Kidney problems: Poor kidney function increases bleeding risk by 2.3 times. Many DOACs are cleared by the kidneys - if they’re not working well, the drug builds up.
- Previous bleeding: If you’ve had a major bleed before, your chance of another one is 4.2 times higher.
- Multiple blood thinners: Taking both an anticoagulant and an antiplatelet (like aspirin or clopidogrel) doubles your risk.
- High drug levels: A 2024 study found that patients with the highest blood levels of DOACs in the first three months had over three times the bleeding risk.

Emergency Response: What to Do When Bleeding Starts
If you notice any of the warning signs, don’t wait. Don’t call your doctor’s office. Don’t wait until morning. Go to the emergency room - now. While you’re on your way:- Stay calm. Panic increases your heart rate and can make bleeding worse.
- Apply direct pressure to any external bleeding. Use a clean cloth or bandage. Keep pressure on for at least 10 minutes without checking.
- Don’t take any more of your blood thinner unless instructed by a doctor.
- Bring your medication list. Include the name, dose, and when you last took it.
- If you’re on warfarin, bring your INR log. If you’re on a DOAC, bring the pill bottle.
Why People Delay - and Why That’s Deadly
A 2023 survey of 1,050 patients found that 37% waited more than two hours before seeking help. Nineteen percent waited over six hours. Why?- They didn’t think it was serious.
- They thought it would stop on its own.
- They were afraid of going to the hospital.
- They didn’t know what counted as an emergency.
Different Drugs, Different Risks
Not all blood thinners are the same. Some are safer than others.- Apixaban: Has the lowest bleeding risk among DOACs. In clinical trials, it caused 2.13% major bleeding per year vs. 3.09% for warfarin. It’s also 31% less likely to cause another GI bleed if you’ve had one before.
- Rivaroxaban: Higher risk of GI bleeding. If you’ve had a stomach ulcer, it’s not the best choice.
- Dabigatran: Slightly higher risk of GI bleeding than apixaban, but easier to reverse with idarucizumab.
- Warfarin: Requires regular blood tests (INR). If your INR is above 3.0, your bleeding risk jumps. But it’s cheaper and has a long history of use.
What You Can Do Before It Happens
Prevention is better than emergency care. Here’s what works:- Get your HAS-BLED score: This simple tool (Hypertension, Abnormal kidney/liver, Stroke, Bleeding history, Lab instability, Elderly, Drugs/alcohol) gives your bleeding risk. A score of 3 or higher means you need extra precautions.
- Ask about DOAC level testing: New point-of-care tests can check your drug levels in minutes. If you’re over 75, have kidney issues, or had a bleed before, ask if this is right for you.
- Review your meds: Are you taking aspirin, NSAIDs (like ibuprofen), or herbal supplements? Many of these increase bleeding risk. Talk to your doctor about cutting them.
- Wear a medical alert bracelet: If you collapse, paramedics need to know you’re on a blood thinner.
- Have a plan: Know the nearest ER. Keep your medication list in your phone and wallet. Tell a family member what to do if you bleed.
The Bigger Picture
More than 4.7 million Americans are on DOACs. That number is rising as the population ages. In 2022, over 128,000 people went to the ER because of bleeding from these drugs - up 27% since 2018. The cost? About $18,500 per major bleeding episode. For brain bleeds, it’s over $52,000. These aren’t just medical costs - they’re lost workdays, caregiver stress, and long-term disability. But there’s hope. New drugs like milvexian and asundexian are in trials and show 20-25% less bleeding than current options. A universal reversal agent called Ciraparantag could be available by 2027. For now, the best defense is knowledge. Know your risk. Know the signs. Know when to act.Can I stop my blood thinner if I start bleeding?
No. Never stop your medication on your own. Stopping suddenly can cause a clot, leading to stroke or heart attack. Instead, go to the ER immediately. Doctors can reverse the drug with specific agents and manage your bleeding safely.
Do all blood thinners cause the same amount of bleeding?
No. Apixaban has the lowest bleeding risk among DOACs. Warfarin requires regular monitoring and can be riskier if your INR is too high. Rivaroxaban carries a higher risk of stomach bleeding. Your doctor chooses based on your history, kidney function, and other medications.
How long after starting a blood thinner am I most at risk?
The first 90 days are the most dangerous. About 60% of major bleeding events happen in this window. This is why close monitoring and patient education are critical during the first few months.
Can I still exercise or be active on blood thinners?
Yes - but be smart. Avoid contact sports, high-risk activities like skiing or rock climbing, and anything where a fall could cause internal bleeding. Walking, swimming, cycling, and light strength training are generally safe. Always wear protective gear if there’s any risk of injury.
What should I do if I forget to take my blood thinner?
If you miss a dose, take it as soon as you remember - but only if it’s within a few hours. If it’s close to your next dose, skip the missed one. Never double up. If you’re unsure, call your doctor or pharmacist. Missing doses increases clot risk, but taking too much increases bleeding risk.
Are there any foods or supplements I should avoid?
If you’re on warfarin, avoid large changes in vitamin K intake (found in leafy greens like kale and spinach). For DOACs, diet matters less - but avoid herbal supplements like ginkgo, garlic, ginger, and fish oil, which can increase bleeding. Always check with your doctor before starting any new supplement.

Mussin Machhour
December 25, 2025 AT 05:48Man, I was on rivaroxaban for AFib last year and almost ignored a nosebleed that lasted 20 minutes. Thought it was just dry air. Ended up in the ER with hemoglobin at 8.2. Lesson learned: if it won’t stop, go now. No excuses.
Terry Free
December 26, 2025 AT 11:54So let me get this straight - we’re paying $12,500 for a drug that reverses another drug we were told was ‘safer’ than warfarin? Brilliant. Just brilliant. Capitalism at its finest.
Justin James
December 27, 2025 AT 12:57Ever wonder why these drugs are pushed so hard? Big Pharma knows people will bleed. They know the ER visits will happen. They know reversal agents cost more than a used car. They don’t care. They’ve got patents, lobbyists, and a 20% profit margin on every pill. The ‘safer’ DOACs? They’re just newer, more expensive ways to bleed out. And the FDA? They’re just the gatekeepers. Wake up.
Rick Kimberly
December 28, 2025 AT 13:09This is one of the most clinically grounded pieces I’ve read on anticoagulant risks. The emphasis on the first 90 days is critical - it’s not just about dosage titration, it’s about neurocognitive adaptation. Patients often misinterpret minor bruising as ‘normal’ when it’s actually a red flag for cumulative pharmacokinetic drift. The HAS-BLED score should be mandatory at prescription.
Lindsay Hensel
December 29, 2025 AT 11:03To anyone reading this: if you’re on a blood thinner, please tell someone - a neighbor, a friend, your kid - what to do if you collapse. I lost my dad to a silent brain bleed because he never told anyone he was on apixaban. No bracelet. No list. Just silence. Don’t let that be you.
Michael Dillon
December 30, 2025 AT 18:56Apixaban’s the best. Low bleeding risk, no INR tests, and you can still drink beer. I’ve been on it 3 years. No bruises, no ER trips. Just take it like your life depends on it - because it does.
Zabihullah Saleh
January 1, 2026 AT 02:57It’s funny how we treat medicine like a math problem - take pill, get result. But the body isn’t a spreadsheet. It’s a messy, aging, stressed-out system trying to survive on caffeine, stress, and 4 hours of sleep. The real issue isn’t the drug - it’s that we’re prescribing life-altering meds to people who don’t have time, money, or support to manage them. We treat the clot, not the person.
Bailey Adkison
January 1, 2026 AT 15:19Anyone who says they 'didn’t know' bleeding was an emergency is either lying or dangerously uninformed. This isn’t rocket science. Black stool? Blood in pee? Headache with no cause? Go to the ER. No ifs ands or buts. Your life isn’t a guessing game. Stop making excuses and start taking responsibility.
Sophie Stallkind
January 2, 2026 AT 22:46While the clinical information presented is both accurate and vital, I must emphasize the profound ethical obligation healthcare providers bear in ensuring patient comprehension. It is not sufficient to merely distribute educational pamphlets; true informed consent necessitates personalized, repeated, and linguistically appropriate dialogue. The data on delayed care underscores a systemic failure in communication, not patient negligence.
Gary Hartung
January 4, 2026 AT 21:01And yet… here we are. Another article telling us to ‘know the signs’ - while the same system that wrote the article also denies us access to affordable labs, forces us to wait 6 weeks for a specialist, and charges $800 for a simple INR test. Knowledge is power? No. Knowledge is a luxury. And I’m tired of being told to ‘be proactive’ when my insurance won’t cover the tools to be proactive.
Ben Harris
January 6, 2026 AT 05:10My uncle took apixaban and started bleeding internally after a fall. They didn’t find it for 3 days because he didn’t want to ‘bother’ anyone. He’s fine now but he walks with a cane because his knee got destroyed from the hematoma. You think this is just about pills? No. It’s about pride. It’s about silence. It’s about being too scared to say ‘I need help.’
Oluwatosin Ayodele
January 6, 2026 AT 06:52In Nigeria, we don’t have reversal agents. We don’t have DOACs. We have warfarin and a 1000 naira note. If you bleed, you pray. If you survive, you’re lucky. This article reads like a luxury pamphlet from a country that doesn’t know what real healthcare access means. Stop preaching to the privileged.
Jason Jasper
January 6, 2026 AT 13:48I’ve been on rivaroxaban for 5 years. I got a point-of-care test done last year - turned out my levels were spiking because I started taking turmeric. No one told me it could interfere. I’m glad I asked. Simple questions save lives.
Carlos Narvaez
January 7, 2026 AT 20:11Apixaban is the only DOAC worth taking. The rest are overpriced gamble. And if you’re on warfarin, you’re either old-school or broke. Either way - respect.