Why Losing Weight Feels Impossible with PCOS
If you have PCOS and have tried every diet out there-keto, intermittent fasting, low-fat, calorie counting-and still can’t shift the weight, you’re not failing. You’re fighting a biological system that’s working against you. The problem isn’t willpower. It’s insulin resistance.
Polycystic Ovary Syndrome (PCOS) isn’t just about irregular periods or acne. At its core, it’s a metabolic disorder. Up to 95% of women with PCOS who are overweight, and as many as 75% of those who aren’t, have insulin resistance. That means your body can’t use insulin properly. Instead of glucose being absorbed by your muscles and organs, it stays in your blood. Your pancreas pumps out more insulin to compensate. And that extra insulin? It’s the hidden driver behind your weight gain, cravings, and stubborn belly fat.
How Insulin Resistance Turns Fat Storage On
Insulin isn’t just a blood sugar regulator. It’s your body’s main fat-storage hormone. When insulin stays high-like it does in PCOS-it does three things that make weight loss nearly impossible:
- It tells your body to store fat, especially around your abdomen.
- It blocks your body from burning stored fat for energy.
- It makes you hungrier, especially for sugary, starchy foods.
This isn’t normal hunger. It’s a biological craving fueled by blood sugar spikes and crashes. You eat a bowl of pasta or a bagel, your blood sugar rockets up, your body dumps out insulin to bring it down-and then it drops too low. That’s when you feel shaky, tired, and suddenly obsessed with a donut. It’s not weakness. It’s biochemistry.
High insulin also lowers a hormone called SHBG, which normally keeps male hormones like testosterone in check. When SHBG drops, testosterone rises. That’s why women with PCOS often gain weight in an ‘apple shape’-around the waist-instead of the more typical ‘pear shape’ in the hips and thighs. Abdominal fat isn’t just cosmetic. It’s metabolically active, releasing inflammatory chemicals that make insulin resistance worse, creating a vicious cycle.
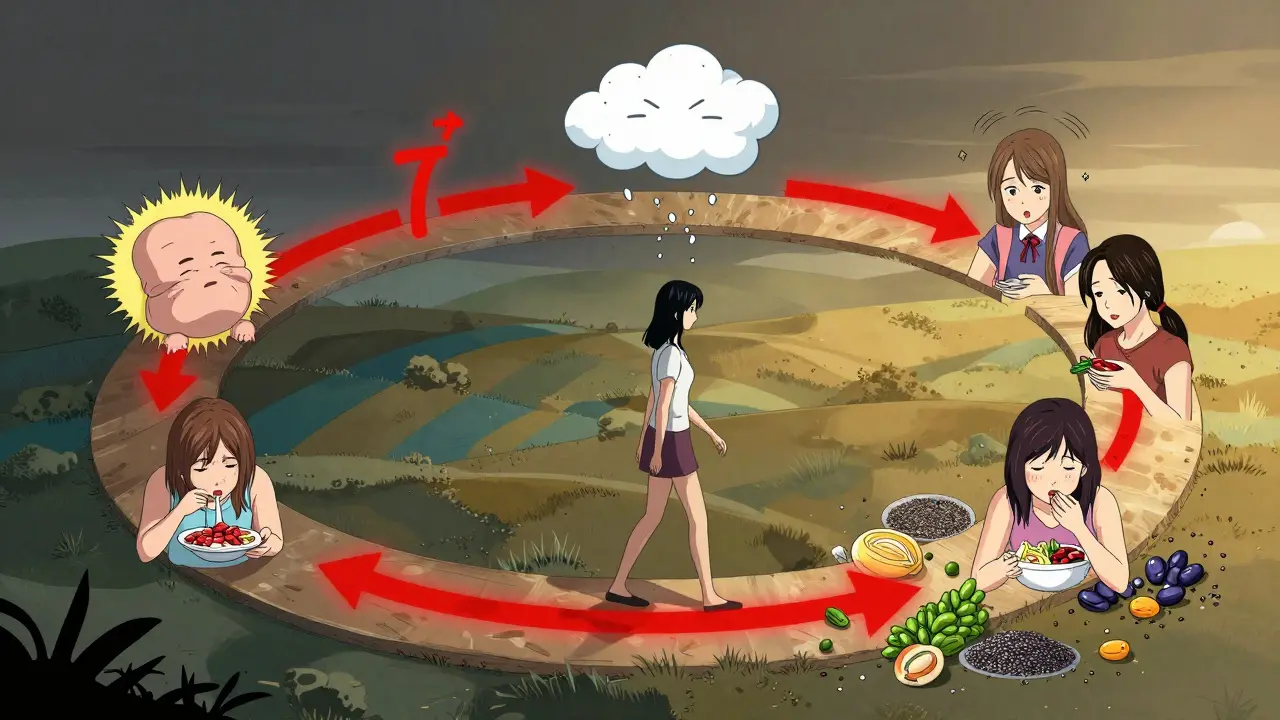
The Cycle That Keeps Getting Worse
Here’s how it loops:
- Insulin resistance → higher insulin → more fat storage
- More fat (especially belly fat) → more insulin resistance
- Higher insulin → more testosterone → worse PCOS symptoms
- Worse symptoms → more stress → more emotional eating
- Emotional eating → blood sugar spikes → more insulin
It’s not a matter of eating too much. It’s a matter of what your body does with what you eat. A 2022 review in PMC found that insulin resistance is the most significant biological trait in PCOS-not just a side effect. That means if you don’t fix insulin, you won’t fix the weight. And if you don’t fix the weight, your insulin resistance gets worse.
That’s why doctors see PCOS as a gateway to type 2 diabetes. The CDC reports that women with PCOS are up to seven times more likely to develop diabetes than women without it. And the risk skyrockets if you’re carrying extra weight. High blood pressure, cholesterol problems, sleep apnea, and even endometrial cancer are all more common in women with PCOS who struggle with insulin resistance.
What to Eat: The Real PCOS Diet
There’s no magic PCOS diet. But there are proven eating patterns that work because they target insulin resistance directly.
1. Cut refined carbs and sugars.
White bread, pasta, rice, pastries, soda, candy-they’re the biggest triggers for insulin spikes. You don’t need to eliminate carbs entirely, but you need to choose ones that don’t spike your blood sugar. Swap white rice for quinoa or barley. Swap regular pasta for lentil or chickpea pasta. Swap sugary cereal for plain oats with berries and nuts.
2. Prioritize protein and healthy fats at every meal.
Protein slows down digestion and keeps insulin steady. Fats help you feel full and reduce cravings. Start your day with eggs and avocado. Have grilled chicken or tofu with broccoli and olive oil for lunch. Snack on Greek yogurt with chia seeds or a handful of almonds.
3. Eat fiber like it’s your job.
Fiber-especially soluble fiber-slows sugar absorption and helps balance insulin. Think beans, lentils, Brussels sprouts, apples with skin, flaxseeds, and chia seeds. Aim for at least 30 grams a day. A 2023 study showed that women with PCOS who increased fiber intake saw better insulin sensitivity and reduced androgen levels.
4. Don’t skip meals.
Skipping meals leads to blood sugar crashes, which trigger intense cravings and overeating later. Eat regular, balanced meals-even if you’re not hungry. Your body needs stability.
5. Avoid processed foods.
They’re loaded with hidden sugars, unhealthy fats, and additives that worsen inflammation and insulin resistance. Read labels. If it has more than five ingredients you can’t pronounce, leave it on the shelf.
What About Low-Carb or Keto?
Many women with PCOS find success with low-carb or even ketogenic diets because they directly lower insulin. A 2022 study showed that a low-carb diet improved ovulation rates and reduced testosterone levels in women with PCOS. But you don’t need to go all-in on keto to see results. Even reducing carbs to 40-45% of your daily calories-instead of the typical 60%-can make a big difference.
The key is sustainability. If cutting carbs feels too extreme, start by removing one high-sugar item per week. Replace it with a protein-rich alternative. Progress, not perfection, is what matters.
Why Weight Loss Is Slower-And That’s Okay
With PCOS, losing even 5-10% of your body weight can dramatically improve symptoms. That’s not a lot. For someone who weighs 200 pounds, that’s just 10-20 pounds. But it’s enough to restart ovulation, lower insulin, reduce acne, and improve mood.
Don’t compare your progress to someone without PCOS. Your body is working harder. Focus on how you feel-not just the number on the scale. Better sleep. More energy. Fewer cravings. Regular periods. These are wins.
Research from the Cleveland Clinic confirms that even small weight loss improves insulin sensitivity and reduces the risk of diabetes. The goal isn’t to be thin. It’s to be metabolically healthy.
Supplements and Medications: Helpful, Not Magic
Metformin, a diabetes drug, is often prescribed for PCOS because it improves insulin sensitivity. Many women report fewer cravings and better weight control on it. But it’s not a substitute for diet. It’s a tool to help you stick to it.
Supplements like inositol (particularly myo-inositol and D-chiro-inositol) have been shown in multiple studies to improve insulin response and reduce testosterone in women with PCOS. Magnesium and vitamin D also help with insulin sensitivity. But again-these work best alongside food changes, not instead of them.

It’s Not Just About Food
Stress raises cortisol, which increases belly fat and worsens insulin resistance. Sleep deprivation does the same. If you’re not sleeping well or you’re constantly stressed, no diet will fix it.
Move your body-but don’t overdo it. Intense, long workouts can spike cortisol. Focus on walking, yoga, swimming, or strength training 3-4 times a week. Movement helps insulin work better without adding stress.
And be kind to yourself. The emotional toll of PCOS is real. Feeling like your body is betraying you, battling cravings you can’t control, watching others lose weight easily-it’s exhausting. You’re not broken. Your biology is just different.
What Works: A Real-Life Example
One woman I know, 34, had PCOS for 8 years. She gained 50 pounds, had irregular periods, and was told she’d never get pregnant. She tried every diet. Nothing stuck.
Then she made three changes:
- She stopped drinking soda and juice.
- She ate protein with every meal-eggs for breakfast, chicken for lunch, lentils for dinner.
- She walked 30 minutes after dinner, every day.
Within 6 months, she lost 22 pounds. Her periods came back. Her acne cleared. Her doctor took her off metformin. She didn’t count calories. She didn’t cut out carbs completely. She just stopped feeding the insulin fire.
Final Thought: You’re Not Broken
PCOS isn’t your fault. The weight gain isn’t laziness. The cravings aren’t weakness. They’re symptoms of a hormonal and metabolic imbalance-and that’s fixable.
You don’t need to be perfect. You just need to be consistent. Eat real food. Move gently. Sleep well. Reduce stress. And give your body time to heal.
Every small step you take to lower insulin doesn’t just help you lose weight. It lowers your risk of diabetes, heart disease, and infertility. It gives you back control. And that’s worth more than any number on a scale.
Can you lose weight with PCOS if you’re not overweight?
Yes. Even women with PCOS who are lean can have insulin resistance. The goal isn’t always weight loss-it’s improving insulin sensitivity. A lean woman with PCOS might focus on reducing belly fat, balancing hormones, and preventing future weight gain by eating low-glycemic foods, getting enough protein, and managing stress.
Is intermittent fasting good for PCOS?
Some women with PCOS benefit from intermittent fasting because it gives insulin a break. But it’s not for everyone. If you’re stressed, under-eating, or have a history of disordered eating, it can make symptoms worse. Start with a 12-hour overnight fast (e.g., 7 pm to 7 am) and see how you feel before trying longer windows.
Why do I crave sugar so much with PCOS?
High insulin causes your blood sugar to crash after meals, triggering intense cravings for quick energy-usually sugar. It’s not a lack of willpower. It’s your body trying to fix a blood sugar imbalance. Eating protein and fiber with every meal helps stabilize blood sugar and reduces these crashes over time.
How long does it take to see results from a PCOS diet?
Most women notice reduced cravings and more energy within 2-4 weeks. Weight loss, if it happens, usually starts after 6-8 weeks. Hormonal improvements-like more regular periods or clearer skin-can take 3-6 months. Patience is key. This isn’t a quick fix; it’s a long-term reset.
Should I avoid dairy with PCOS?
There’s no strong evidence that dairy causes PCOS symptoms in everyone. But some women find that full-fat dairy increases androgen levels or inflammation. If you suspect dairy is a trigger, try cutting it out for 4 weeks and see if your skin, cycle, or cravings improve. Choose unsweetened plant-based alternatives if needed.

Melissa Melville
February 1, 2026 AT 17:12vivian papadatu
February 3, 2026 AT 05:20Deep Rank
February 4, 2026 AT 23:28Naomi Walsh
February 4, 2026 AT 23:52Nancy Nino
February 6, 2026 AT 02:10June Richards
February 7, 2026 AT 14:39Jaden Green
February 9, 2026 AT 00:01Lu Gao
February 9, 2026 AT 18:49Angel Fitzpatrick
February 10, 2026 AT 10:00Jamie Allan Brown
February 10, 2026 AT 21:25Nicki Aries
February 11, 2026 AT 22:22Ed Di Cristofaro
February 13, 2026 AT 03:57