When OCD takes over your daily life-making you check the lock ten times, wash your hands until they bleed, or replay conversations in your head for hours-medication isn't just an option. It's often the bridge back to normalcy. But with so many drugs out there, and dosing that doesn’t follow the same rules as depression or anxiety, it’s easy to feel lost. The truth? Only two classes of medication have solid, proven effectiveness for OCD: SSRIs and clomipramine. Everything else is either unproven or used as an add-on. And dosing? It’s not what you think.
Why SSRIs Are the First Step
SSRIs-selective serotonin reuptake inhibitors-are the go-to starting point for OCD treatment. That’s not because they’re perfect. It’s because they’re the safest bet. Fluoxetine, sertraline, paroxetine, fluvoxamine, and escitalopram are all FDA-approved for OCD in adults and, in some cases, children. But here’s the catch: the doses needed for OCD are way higher than what’s used for depression.For depression, you might start with 20 mg of sertraline. For OCD? You’ll likely need to go up to 200-300 mg. Same drug. Totally different goal. The American Psychiatric Association says you need at least 8-12 weeks of treatment at a high dose before deciding if it’s working. Many people give up after 4 weeks because they don’t feel better right away. But OCD doesn’t respond like a cold. It takes time.
Typical starting doses for SSRIs in OCD:
- Fluvoxamine: 25-50 mg/day
- Sertraline: 25 mg/day
- Paroxetine: 20 mg/day
- Fluoxetine: 20 mg/day
From there, doses go up by 25-50 mg every 5-7 days. Most people reach their target dose in 4-6 weeks. The maximums? Fluvoxamine can go up to 300 mg/day. Sertraline to 300 mg. Paroxetine to 60 mg. Fluoxetine to 80 mg. These aren’t random numbers. They’re based on clinical trials showing real improvement in OCD symptoms.
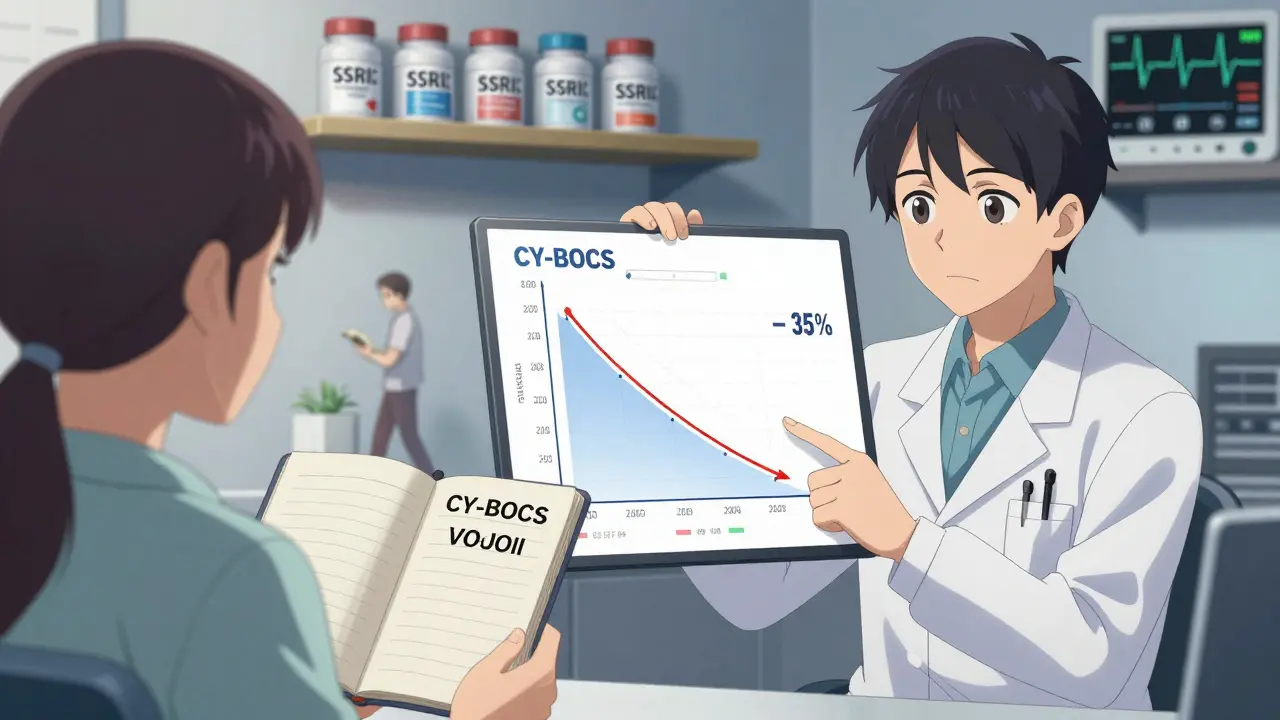
One study found that patients who stayed on sertraline at 200 mg/day for 12 weeks saw a 35% drop in their Yale-Brown Obsessive Compulsive Scale (CY-BOCS) scores-the gold standard for measuring OCD severity. A 25-35% reduction is considered clinically meaningful. That means fewer rituals, less time spent obsessing, and more hours back in your life.
Clomipramine: The Old Guard That Still Works
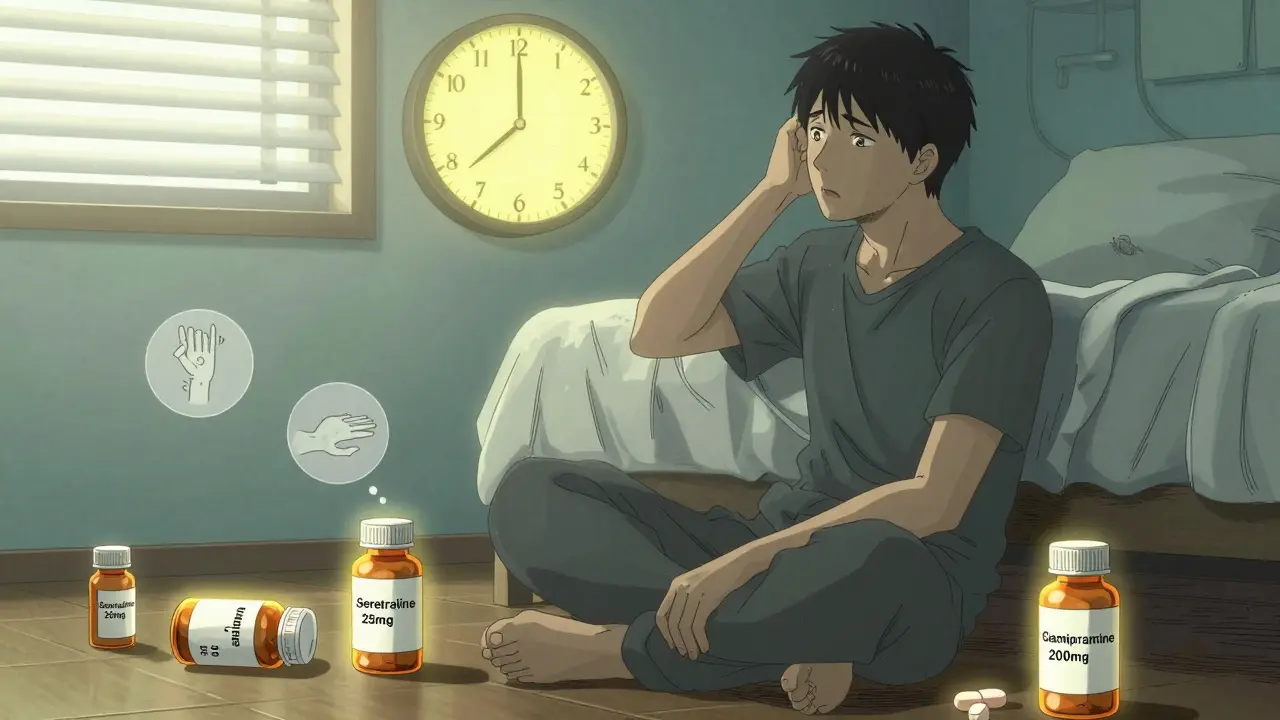
Clomipramine was the first drug ever approved by the FDA specifically for OCD-in 1989. It’s a tricyclic antidepressant, not an SSRI. That means it affects more than just serotonin. It also blocks norepinephrine and has strong anticholinergic effects. That’s why it works. And why it’s so hard to tolerate.Clomipramine is more effective than SSRIs in some cases-especially for people with contamination fears or checking compulsions. One meta-analysis showed it improved CY-BOCS scores by 37% in kids and teens, outperforming sertraline and fluoxetine. For adults, studies show it’s about equal in effectiveness to SSRIs. But here’s the problem: side effects.
Clomipramine causes dry mouth, constipation, blurred vision, weight gain, drowsiness, and heart rhythm changes. In fact, 28% of people stop taking it because of side effects, compared to 15-18% for SSRIs. A Reddit user wrote: “Clomipramine at 175 mg stopped my checking rituals after 5 failed SSRIs. But I was so tired I couldn’t drive.” That’s not uncommon.
Dosing for clomipramine is precise:
- Adults: Start at 25 mg/day. Increase by 25 mg every 4-7 days. Target: 100-250 mg/day. Max: 250 mg/day.
- Children (10+): 1-3 mg/kg/day. Max: 200-250 mg/day depending on guidelines.
- Elderly: Start at 10 mg/day. Usually stay under 50 mg/day.
Most doctors give it at bedtime because of the sedation. Higher doses are often split-150 mg at night, 50 mg in the morning. Blood levels matter too. Responders usually have clomipramine levels between 220-350 ng/mL and desmethylclomipramine (its active metabolite) around 379 ng/mL. That’s why some psychiatrists check blood levels after 6-8 weeks.
Why You Might Skip Clomipramine (and When You Shouldn’t)
Most doctors won’t start you on clomipramine. Not because it doesn’t work. Because it’s risky. It can prolong the QTc interval on an ECG, which raises the chance of dangerous heart rhythms. That’s why you need an ECG before starting if your dose is over 150 mg/day. Liver function tests are also recommended.But here’s what many patients don’t know: clomipramine is often the answer when SSRIs fail. The APA guideline says try two adequate SSRI trials before switching. An adequate trial means 12 weeks at the highest tolerated dose. If you’ve tried sertraline at 200 mg for 3 months and still can’t leave the house without checking the stove 12 times, clomipramine might be your next step.
And it’s not just for people who’ve tried everything. Some experts use it as an add-on. Low-dose clomipramine (25-75 mg/day) combined with an SSRI boosts response rates by 35-40% in people who only partially improve. That’s a big deal. You’re not replacing the SSRI-you’re adding a second tool to the toolbox.
One psychiatrist in Adelaide told me: “I’ve had three patients in the last year who couldn’t tolerate SSRIs but responded beautifully to low-dose clomipramine. One was a teacher who couldn’t grade papers because of intrusive thoughts. After 8 weeks on 50 mg, she was back in the classroom.”
What About Side Effects and Real-Life Trade-Offs?
Side effects aren’t just numbers on a chart. They’re real. On Drugs.com, SSRIs have an average effectiveness rating of 6.8/10 and satisfaction of 6.2/10. Clomipramine? 7.2/10 for effectiveness but only 5.1/10 for satisfaction. Why? Because the side effects eat into your quality of life.People on clomipramine report:
- Drinking 5-6 glasses of water an hour just to deal with dry mouth
- Gaining 15-25 pounds in 6 months
- Feeling like they’re walking through syrup
- Struggling to concentrate at work
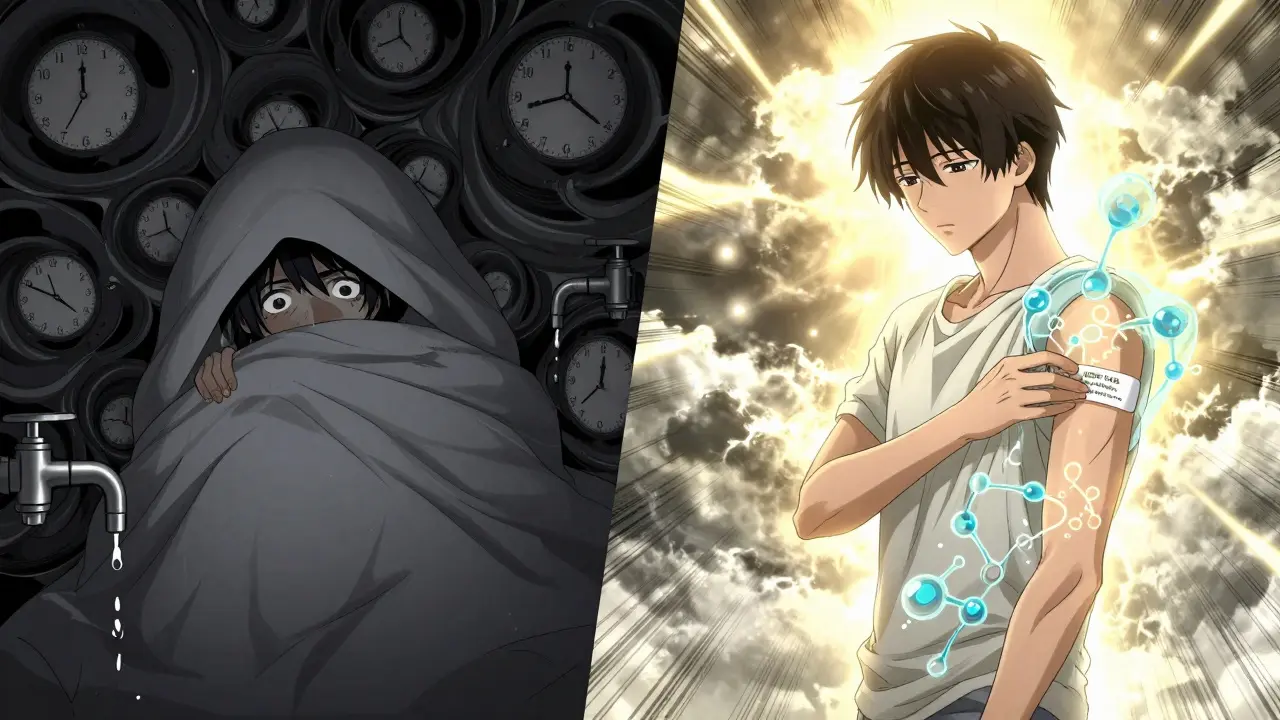
SSRIs have their own issues: nausea, sexual dysfunction, insomnia, and sometimes increased anxiety in the first 1-2 weeks. That’s why some doctors start with ultra-low doses-12.5 mg of sertraline or clomipramine-to avoid the initial spike in anxiety. It’s a small trick, but it helps people stick with treatment.
And here’s something most patients don’t expect: the first 2 weeks can make OCD worse. That’s normal. It’s not a sign the drug isn’t working. It’s the brain adjusting. 89% of people who push through those first two weeks see improvement by week 6. But if no one warns you? You might quit.
How We Know It’s Working
You can’t just guess if your medication is helping. You need to measure it. That’s where the CY-BOCS comes in. It’s a 10-item scale scored by a clinician. It asks about time spent on obsessions, distress caused, resistance efforts, and interference with daily life. A score of 28-31 means severe OCD. 16-23 is moderate. Below 10 is mild.Most people see improvement in 4-8 weeks. But the real test is whether your score drops by 25-35%. If you started at 28 and now you’re at 19? That’s a win. You’re not cured. But you’re not trapped anymore.
Doctors usually check this every 2-4 weeks during the first 3 months. If there’s no change after 12 weeks? Time to adjust. Maybe a higher dose. Maybe a different SSRI. Maybe clomipramine.
What’s Next? The Future of OCD Treatment
SSRIs and clomipramine aren’t the end. New options are coming. In March 2023, the FDA gave Breakthrough Therapy status to SEP-363856, a new serotonin modulator that showed 45% response rates in treatment-resistant OCD. That’s huge.Psilocybin-the active compound in magic mushrooms-is being tested in phase 3 trials with SSRIs. Early results show 60% remission at 6 months, compared to 35% with SSRIs alone. It’s not available yet. But it’s coming.
For clomipramine, researchers are testing a skin patch that delivers the drug slowly. Early results show it works just as well as the pill-but with 40% fewer side effects. That could change everything for people who can’t tolerate the oral version.
Right now, SSRIs are used in 85% of first-line OCD prescriptions. Sertraline leads the pack at 32%. Clomipramine is only 8% of initial prescriptions-but jumps to 22% after two failed SSRI trials. That tells you something: it’s not the first choice. But it’s the best second choice.
What to Do If You’re Starting Medication
If you’re considering medication for OCD, here’s your practical roadmap:- Start with an SSRI. Pick one your doctor recommends-sertraline or fluvoxamine are common first choices.
- Don’t expect results in 2 weeks. Give it 8-12 weeks at the highest dose you can tolerate.
- Track your symptoms with a simple journal. Note how many rituals you do, how much time they take, how much distress they cause.
- If no improvement after 12 weeks, talk to your doctor about switching or adding clomipramine.
- If you try clomipramine, expect side effects. Start low. Go slow. Get an ECG if your dose hits 150 mg or more.
- Don’t quit because of early side effects. Most fade after 2-4 weeks.
- Combine medication with exposure therapy. It’s the most effective combo out there.
Medication doesn’t fix OCD. It gives you the mental space to do the hard work of therapy. And sometimes, that’s enough to get your life back.
Can SSRIs make OCD worse at first?
Yes. In the first 1-2 weeks, some people experience a temporary spike in anxiety or obsessive thoughts. This is common and usually resolves if the medication is continued. About 89% of patients who stick with treatment see improvement by week 6. Starting with a lower dose (like 12.5 mg) can help reduce this initial reaction.
Is clomipramine better than SSRIs for OCD?
Clomipramine is equally effective as SSRIs for adults and slightly more effective in children and teens, especially for contamination fears. But it has significantly more side effects-dry mouth, weight gain, drowsiness, heart rhythm changes-so it’s usually reserved for when SSRIs don’t work. About 28% of people stop clomipramine due to side effects, compared to 15-18% for SSRIs.
How long does it take for OCD medication to work?
It typically takes 8-12 weeks to see full effects. Some improvement may appear after 4-6 weeks, but most guidelines recommend waiting at least 6 weeks at the maximum tolerated dose before deciding if a medication is effective. Patience is critical-OCD responds slowly to medication.
What’s the highest safe dose of sertraline for OCD?
The maximum FDA-approved dose for sertraline in OCD is 200 mg per day. However, many clinicians safely prescribe up to 300 mg per day in treatment-resistant cases, under close monitoring. Studies show doses above 200 mg can offer additional benefit for some patients who don’t respond at lower levels.
Can you take clomipramine and an SSRI together?
Yes. Combining a low dose of clomipramine (25-75 mg/day) with an SSRI is a common and effective strategy for people who only partially respond to SSRIs alone. This approach boosts response rates by 35-40% in treatment-resistant cases. However, this combination requires careful monitoring due to increased risk of serotonin syndrome and heart rhythm changes.
Do I need blood tests or ECGs for OCD meds?
For clomipramine, an ECG is recommended before starting and if the dose exceeds 150 mg/day due to risk of QTc prolongation. Liver function tests are also advised. Blood level monitoring (for clomipramine and its metabolite) is not routine but can be helpful in treatment-resistant cases or when side effects are severe. SSRIs generally don’t require routine blood tests unless there are other health concerns.
Randolph Rickman
December 15, 2025 AT 12:50Just wanted to say this is the most clear, practical guide to OCD meds I've ever read. I tried sertraline for 6 months at 150mg and thought it wasn't working until my therapist reminded me to wait for 12 weeks at full dose. Turned out I was down from 4 hours of rituals to 45 minutes. Small win, but life-changing. Keep pushing through the fog.
sue spark
December 17, 2025 AT 12:42I started on fluvoxamine at 25mg and my doctor wanted to go up fast but I begged for slower. Took 3 months to get to 100mg. The first 2 weeks were hell but I didn't quit. Now I can sleep through the night without checking the door 17 times. Patience is the real medicine.
James Rayner
December 18, 2025 AT 15:22There's something deeply human about how OCD meds work-not by erasing thoughts, but by giving you the space to let them pass like clouds. Clomipramine didn't fix me, but it gave me the quiet mind to finally do the exposure work I'd been avoiding for years. It's not a cure. It's a doorway. And sometimes, that's all you need.
I remember sitting in my car after my first 12-week check-in, just breathing. No rituals. No counting. Just air. That's when I realized: I wasn't healed. But I was free enough to start healing.
The side effects? Yeah, they're brutal. Dry mouth so bad I kept a water bottle taped to my steering wheel. Weight gain that made me avoid mirrors. But none of that compared to the weight of the obsession.
People say 'just think differently.' But you can't think your way out of a brain wired to scream danger when there's none. Medication doesn't change your thoughts. It changes how loud they are.
I wish someone had told me that earlier. Not that meds are magic. But that they're the scaffolding. The real work? That's yours. And you're not alone in doing it.
Also-yes, the first two weeks suck. I cried every day. But I kept taking it. And on day 14? My hand stopped hovering over the light switch. Just… stopped. Like a muscle memory broke. That’s when I knew.
To everyone on the edge of quitting: stay. The brain doesn't heal on your schedule. It heals on its own. And it's slower than you think. But it's worth it.
And to the doctors reading this: thank you for knowing the doses. For not giving up on us. For knowing 200mg of sertraline isn't 'too much.' It's exactly right.
Josias Ariel Mahlangu
December 18, 2025 AT 21:12Why are we medicating people instead of teaching them discipline? This is just weakness dressed up as science. My grandfather fought in the war and never took a pill for anxiety. He just got up and did what needed doing. We’ve become a nation of patients instead of people.
Andrew Sychev
December 20, 2025 AT 15:09THIS IS WHY I HATE PSYCHIATRY. SSRIs are just chemical lobotomies. They turn you into a zombie so you stop caring about your obsessions instead of fixing the root cause. And now they want to give us magic mushrooms? Next they'll be injecting you with government nanobots to 'regulate your thoughts.' I know what they're really doing.
Kim Hines
December 22, 2025 AT 00:07I’ve been on clomipramine for 8 months. Still get dry mouth like I’m chewing cotton. But I can finally sit in a meeting without mentally redoing every sentence I said. Worth it.
Cassandra Collins
December 22, 2025 AT 20:20Did you know the FDA is hiding the truth about SSRIs? They’re linked to the rise in mass shootings because they make people detached and numb. My cousin took sertraline and then… well you know what happened. They don’t want you to know this. But I do. And now you do too.
Dylan Smith
December 23, 2025 AT 13:07I was on 200mg sertraline for 10 weeks with zero progress so I added 50mg clomipramine. Within 3 weeks my CY-BOCS dropped from 29 to 18. My therapist was shocked. I didn’t even tell her I added it until the numbers spoke for themselves. If you’re stuck, don’t be afraid to combine. Just do it with a doctor who knows their stuff.
Mike Smith
December 25, 2025 AT 10:22Thank you for writing this with such clarity and compassion. As a clinician, I see too many patients abandon treatment because they believe they’re failing when the medication hasn’t had time to work. Your breakdown of dosing timelines and expectations is exactly what the community needs. I will be sharing this with every new patient I see. You’ve turned complex science into human hope.
Ron Williams
December 25, 2025 AT 14:54As someone who grew up in a culture where mental health was never discussed, I didn’t even know OCD could be treated. I thought I was just ‘overly careful.’ Finding this info changed everything. I’m now on sertraline and going to therapy. I’m not ‘broken.’ I’m healing. Thank you for normalizing this.
Colleen Bigelow
December 26, 2025 AT 10:37Who’s funding these studies? Big Pharma? The FDA? The CDC? You think they really care about your mental health? Or are they just selling pills to keep you docile while they control the system? Clomipramine? That’s just the old-school version of the same poison. They don’t want you cured. They want you dependent. Wake up.