UTI Antibiotic Comparison Tool
Key UTI Treatment Criteria
- Spectrum of Activity: Ability to kill common uropathogens
- Pharmacokinetics: Achieves high concentrations in bladder
- Resistance Rates: Local bacterial resistance patterns
- Side Effect Profile: Serious or frequent adverse reactions
- Safety: Kidney and pregnancy considerations
- Cost & Convenience: Therapy duration and pill burden
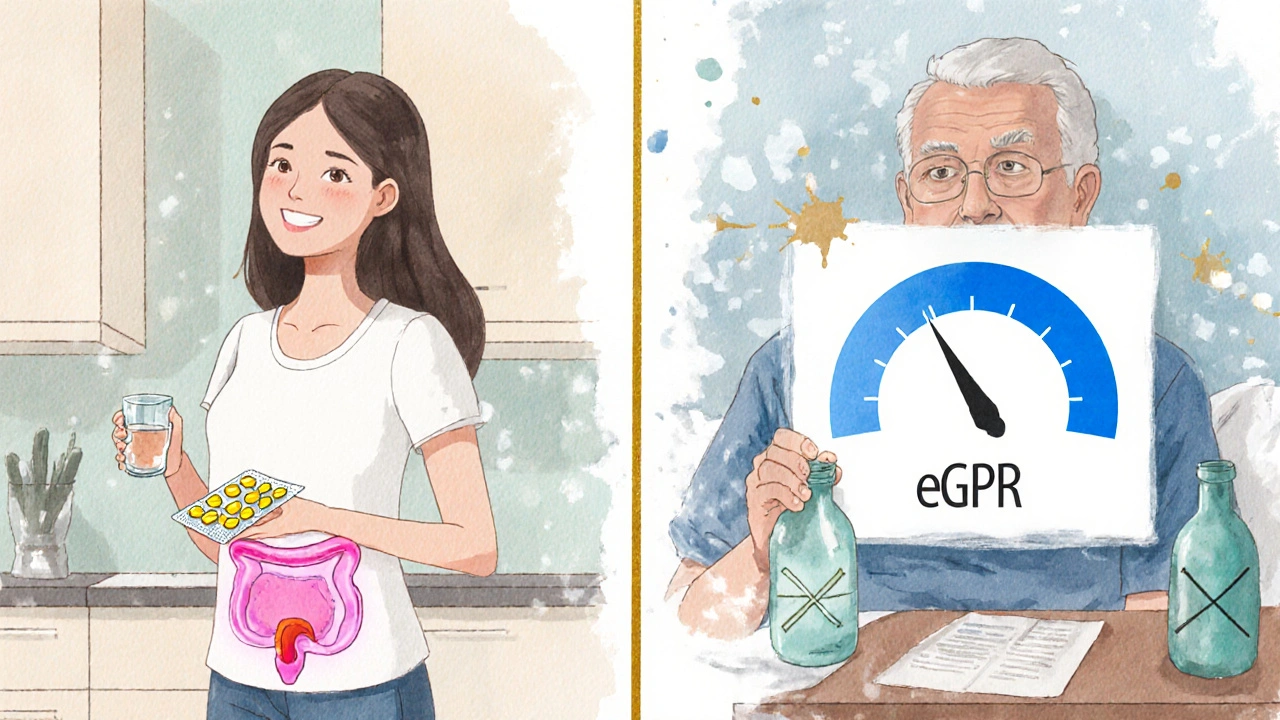
When it comes to treating uncomplicated urinary tract infections (UTIs), Nitrofurantoin is a synthetic nitrofuran antibiotic that concentrates in urine and kills common uropathogens like Escherichia coli. It’s been a go‑to drug for decades because it’s cheap, works well, and has a low impact on gut flora. But rising resistance, kidney‑function limits, and patient‑specific concerns mean doctors and patients often ask: what are the viable nitrofurantoin alternatives?
What makes a good UTI antibiotic?
Before we compare drugs, let’s outline the key criteria clinicians use when picking a UTI treatment:
- Spectrum of activity - ability to kill the most common uropathogens.
- Pharmacokinetics - does the drug achieve high concentrations in the bladder?
- Resistance rates - how often do local bacteria resist the drug?
- Side‑effect profile - any serious or frequent adverse reactions?
- Kidney and pregnancy safety - important for many patients.
- Cost and convenience - duration of therapy and pill burden.
Top alternatives to Nitrofurantoin
Below are the most frequently considered alternatives, each introduced with a brief definition and key attributes.
Trimethoprim‑sulfamethoxazole is a combined sulfonamide that blocks bacterial folic‑acid synthesis, widely used for many infections including UTIs. It’s often called TMP‑SMX or co‑trimoxazole.
Fosfomycin is a phosphonic acid antibiotic that interferes with bacterial cell‑wall formation, administered as a single oral dose for uncomplicated UTIs.
Ciprofloxacin is a fluoroquinolone that inhibits bacterial DNA gyrase, offering broad‑spectrum coverage but with notable safety warnings.
Amoxicillin‑clavulanate is a beta‑lactam/beta‑lactamase inhibitor combo that expands amoxicillin’s spectrum to include many resistant strains.
Side‑effect snapshot
Every antibiotic carries risks. Here’s a quick look at the most common adverse events for each drug:
- Nitrofurantoin - pulmonary toxicity (rare), peripheral neuropathy, gastrointestinal upset.
- Trimethoprim‑sulfamethoxazole - rash, hypersensitivity, possible kidney crystal formation, increased serum potassium.
- Fosfomycin - mild diarrhea, rare allergic reactions.
- Ciprofloxacin - tendon rupture, QT prolongation, CNS effects (dizziness, confusion).
- Amoxicillin‑clavulanate - diarrhea (often due to Clostridioides difficile), liver enzyme elevation.
Comparative table
| Drug | Mechanism | Typical Dose & Duration | Efficacy (uncomplicated UTI) | Resistance Rate (US, 2023) | Major Side Effects | Contraindications | Cost (AU$) |
|---|---|---|---|---|---|---|---|
| Nitrofurantoin | DNA damage via nitro‑reduction | 100mg BID for 5‑7days | ≈85‑90% | ≈10% E.coli resistance | Pulmonary toxicity, neuropathy | eGFR <30mL/min, pregnancy (first trimester) | ≈$8 |
| Trimethoprim‑sulfamethoxazole | Folic‑acid synthesis blockade | 800/160mg BID for 3days | ≈80‑85% | ≈15% E.coli resistance | Rash, hyperkalemia, crystal nephropathy | Renal insufficiency, sulfa allergy, pregnancy (first trimester) | ≈$12 |
| Fosfomycin | Cell‑wall synthesis inhibition | 3g single dose | ≈78‑82% | ≈5‑7% resistance (regional) | Diarrhea, rare allergic reaction | Severe renal impairment (eGFR <30mL/min) | ≈$20 |
| Ciprofloxacin | DNA gyrase inhibition | 250mg BID for 3days | ≈88‑92% | ≈12% resistance in community isolates | Tendon rupture, QT prolongation | Pregnancy, children <18y, history of tendinopathy | ≈$15 |
| Amoxicillin‑clavulanate | Beta‑lactam + beta‑lactamase inhibition | 500/125mg TID for 5‑7days | ≈70‑75% | ≈20% resistance (beta‑lactamase producers) | Diarrhea, liver enzyme rise | Liver disease, known beta‑lactam allergy | ≈$10 |
How to choose the right option
Imagine you’re a 30‑year‑old woman with a first‑time UTI, normal kidney function, and no drug allergies. Nitrofurantoin is usually the first pick because it’s cheap and has low collateral damage. But if your local lab reports a high nitrofurantoin resistance rate, the next best bet is often fosfomycin - a single‑dose convenience that bypasses resistance.
Now picture a 68‑year‑old man with chronic kidney disease (eGFR 28mL/min). Nitrofurantoin isn’t safe, and fosfomycin may also be contraindicated. In that case, a short course of trimethoprim‑sulfamethoxazole (if no sulfa allergy) or a carefully monitored dose of ciprofloxacin can be used, keeping an eye on potential tendon issues.
Key decision steps:
- Check local susceptibility data (often available from your clinic’s lab).
- Assess kidney function - eGFR <30mL/min rules out nitrofurantoin and fosfomycin.
- Identify pregnancy status or sulfa allergy - switch away from TMP‑SMX if needed.
- Consider cost and dosing convenience - a singledose vs a 5‑day regimen.
- Review patient history for tendon or liver concerns before choosing ciprofloxacin or amoxicillin‑clavulanate.
Special populations
Pregnancy: Nitrofurantoin is generally safe after the first trimester, but avoided in early pregnancy due to rare hemolytic anemia risk. Fosfomycin has limited data but is often used in the third trimester. TMP‑SMX is contraindicated in the first trimester and near term because of kernicterus risk.
Elderly patients: Reduced renal clearance pushes clinicians toward agents with safer profiles in low eGFR, like cefpodoxime (not listed above) or low‑dose fluoroquinolones, but watch for drug‑drug interactions.
Patients with recurrent UTIs: A prophylactic low‑dose nitrofurantoin (50mg nightly) is common, but if resistance emerges, rotating to fosfomycin every few months can keep bacteria off‑balance.
Cost and access in Australia
In 2025, the Pharmaceutical Benefits Scheme (PBS) continues to list nitrofurantoin as a low‑cost option ( Nitrofurantoin works best for uncomplicated UTIs when the patient has normal kidney function (eGFR≥30mL/min), no known sulfa or nitro‑fingerprint allergy, and the local bacteria are still sensitive. Its narrow spectrum also means fewer gut‑flora disruptions. Switch to an agent with a lower resistance rate, such as fosfomycin (single‑dose) or trimethoprim‑sulfamethoxazole if the patient isn’t allergic. In areas with high fluoroquinolone resistance, consider amoxicillin‑clavulanate or a tailored therapy based on susceptibility. It’s generally avoided in the first trimester due to rare hemolytic anemia risk. After 13weeks, many obstetric guidelines accept it, but clinicians still monitor the baby’s bilirubin levels. Fosfomycin can be used later in pregnancy when needed. If eGFR drops below 30mL/min, nitrofurantoin doesn’t reach therapeutic urine concentrations and should be avoided. Alternatives like trimethoprim‑sulfamethoxazole (dose‑adjusted) or a fluoroquinolone may be safer, pending other risk factors. Fosfomycin’s production cost, patented formulation, and lack of PBS subsidy keep its price higher. However, the convenience of a single‑dose regimen can offset indirect costs like missed work days. Choosing the right UTI antibiotic hinges on three pillars: local resistance patterns, patient‑specific safety factors, and practical considerations like cost and dosing frequency. Nitrofurantoin remains a solid first‑line choice for most healthy adults, but alternatives such as fosfomycin, trimethoprim‑sulfamethoxazole, ciprofloxacin, and amoxicillin‑clavulanate fill the gaps when nitrofurantoin isn’t suitable. By running through the quick checklist and weighing the table’s data, you can land on a therapy that clears the infection without unwanted side effects.Quick reference checklist
Frequently Asked Questions
Frequently Asked Questions
When should I use nitrofurantoin instead of other antibiotics?
What if my urine culture shows nitrofurantoin resistance?
Is nitrofurantoin safe during pregnancy?
Can I take nitrofurantoin if I have chronic kidney disease?
Why is fosfomycin so expensive compared to nitrofurantoin?
Bottom line

Paige Crippen
October 4, 2025 AT 12:50Ever wonder why Nitrofurantoin is pushed as the go‑to UTI drug? The big pharma lobbyists have a vested interest in keeping us on cheap, old antibiotics while the newer, patented ones get all the hype. They hide the real resistance numbers and whisper about side effects only in the fine print. It’s all part of the grand scheme to keep us dependent on their endless supply.
sweta siddu
October 4, 2025 AT 14:13Hey folks! 😊 This comparison tool is super helpful – love how it breaks down spectrum, resistance, and side‑effects in one place! If you’re juggling a busy schedule, the convenience factor (pill count, duration) is a game‑changer. And those emojis make the data feel less intimidating. Keep it up! 🙌
Ted Mann
October 4, 2025 AT 15:36When we stare into the abyss of bacterial resistance, we confront the paradox of choice. Nitrofurantoin appears elegant, a simple molecule that dares to assault uropathogens, yet its specter looms over renal function. The true tragedy is not the drug itself but the complacency of a system that treats antibiotics as interchangeable toys. We must interrogate not just efficacy percentages, but the philosophical cost of our collective surrender to a pharmacological status quo.
Brennan Loveless
October 4, 2025 AT 17:00Patriots, listen up – the ‘best’ UTI meds often come from overseas labs that don’t share our values. We should champion home‑grown antibiotics that respect American kidneys and keep our soldiers healthy. Nitrofurantoin may work, but it’s a foreign import; why not support domestic research for alternatives that align with our national health agenda?
Vani Prasanth
October 4, 2025 AT 18:23Great points, Ted. Let’s remember that patient education is key. If we can walk someone through how Nitrofurantoin concentrates in the bladder and why it’s relatively safe in pregnancy, they’ll feel empowered to follow the regimen correctly. A supportive coach can demystify side‑effects and improve adherence – that’s where real impact lies.
Maggie Hewitt
October 4, 2025 AT 19:46Oh wow, another "miracle" drug list. Because nothing says "trustworthy" like a glowing chart with no mention of the rare but scary pulmonary toxicity. Sure, it’s cheap and short‑course, but let’s not pretend the side‑effects aren’t real. Sarcasm aside, always read the fine print.
Shaquel Jackson
October 4, 2025 AT 21:10Meh, looks fine.
Tom Bon
October 4, 2025 AT 22:33I appreciate the thoroughness of this tool. The categorization of pharmacokinetics alongside resistance data provides a clear framework for clinicians. It is a commendable effort to present complex information in an accessible format while maintaining a professional tone.
Clara Walker
October 4, 2025 AT 23:56Let’s not overlook the hidden agenda behind these “neutral” presentations. The powers that be prefer drugs that keep the population under surveillance, and Nitrofurantoin is just a pawn. If you’re truly looking for the best choice, consider the geopolitical motives that shape drug approvals.
Jana Winter
October 5, 2025 AT 01:20Firstly, “its” should be “it’s” when you’re contracting "it is". Secondly, the phrase "the tool is super helpful" is overly casual for a medical context. Lastly, avoid the cliché "keep it up" – it adds nothing substantive. Please proofread before posting.
Linda Lavender
October 5, 2025 AT 02:43Ah, the grand tapestry of urinary tract infection pharmacotherapy unfurls before us, a veritable opera of microbial warfare wherein Nitrofurantoin, Trimethoprim‑Sulfamethoxazole, Fosfomycin, Ciprofloxacin, and Amoxicillin‑Clavulanate each claim a solitary spotlight on the stage of the human bladder. First, let us consider the ancient hero, Nitrofurantoin, whose mechanism of DNA damage via nitro‑reduction has long been lauded for its bladder‑specific concentration, yet its shadowed side‑effects – pulmonary toxicity, neuropathy, and gastrointestinal upset – loom like a tragic chorus. Second, the sulfa‑based Trimethoprim‑Sulfamethoxazole, a stalwart of the 20th century, offers broad‑spectrum activity, but the rising tide of resistance (now hovering near 20% in many locales) whispers a cautionary tale of overuse. Third, Fosfomycin, the newcomer with a single‑dose regimen, dazzles with convenience, though cost may impede its ubiquity in everyday practice. Fourth, the fluoroquinolone Ciprofloxacin, once the darling of clinicians, now suffers a tarnished reputation due to collateral damage to tendons and the unsettling specter of Clostridioides difficile. Fifth, Amoxicillin‑Clavulanate, a broad‑spectrum juggernaut, brings its own baggage of hepatotoxicity and the ever‑present risk of fostering resistant flora. Moreover, the pharmacokinetic tableau reveals that only Nitrofurantoin and Fosfomycin achieve the coveted high urinary concentrations, a fact that cannot be ignored when selecting a regimen for uncomplicated cystitis. The resistance landscape further complicates the equation, as local antibiograms dictate the nuanced choice between a tried‑and‑true agent and an emerging alternative. Safety considerations, particularly in populations with compromised renal function or in pregnancy, demand that we scrutinize eGFR thresholds before prescribing Nitrofurantoin, while the teratogenic potential of sulfonamides calls for vigilance. Cost, indeed, remains a decisive factor for many patients; a five‑day Nitrofurantoin course may be economical, yet a single dose of Fosfomycin, though pricier, may save money in the long run by reducing missed work days. In conclusion, the clinician stands at a crossroads, balancing efficacy, resistance patterns, side‑effect profiles, safety, and economics, all while navigating the ever‑shifting sands of microbial evolution; the choice, dear reader, is never truly simple, but this tool provides a compass to guide us through the labyrinthine world of UTI treatment.
Jay Ram
October 5, 2025 AT 04:06Team, let’s keep the momentum going! Even if the data feels overwhelming, remember every correct prescription is a win for public health. Stay curious, stay compassionate, and keep empowering patients with the knowledge they deserve.