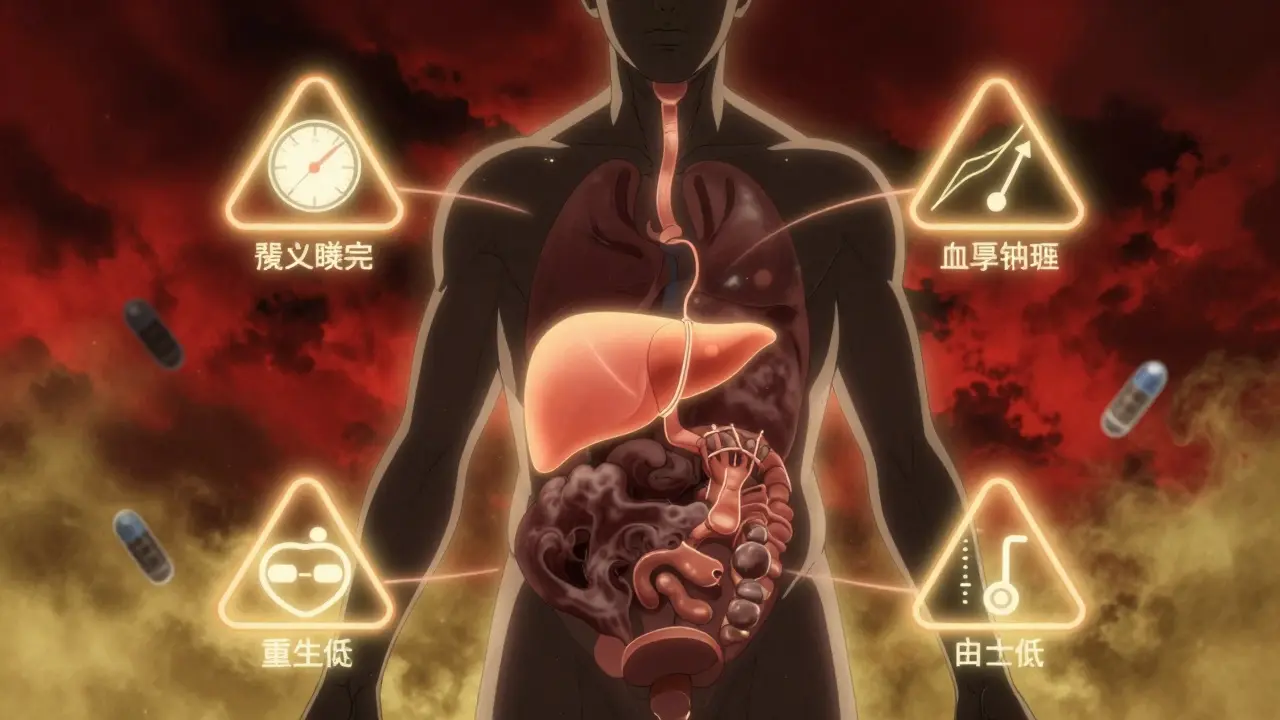
More than 86 million adults in the U.S. have a condition that silently raises their risk of heart attack, stroke, and type 2 diabetes - and many don’t even know it. This isn’t one single problem. It’s a cluster of five warning signs that show up together: too much belly fat, high blood pressure, bad cholesterol levels, and rising blood sugar. Together, they form metabolic syndrome, a red flag that your body’s metabolism is out of balance - and your heart is in danger.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a disease you can point to on a scan. It’s a pattern - a group of physical changes that happen at the same time because your body isn’t responding properly to insulin. Insulin is the hormone that tells your cells to take in sugar from your blood. When your cells start ignoring insulin, your pancreas pumps out more and more to compensate. That extra insulin doesn’t just raise blood sugar - it also triggers fat storage, raises blood pressure, and messes with your cholesterol.
The American Heart Association and the National Heart, Lung, and Blood Institute say you have metabolic syndrome if you have at least three of these five criteria:
- Abdominal obesity: Waist size over 40 inches for men, or 35 inches for women (lower for Asian Americans: 35 inches for men, 31 inches for women)
- High triglycerides: 150 mg/dL or higher
- Low HDL (good) cholesterol: Below 40 mg/dL for men, below 50 mg/dL for women
- High blood pressure: 130/85 mmHg or higher
- Elevated fasting blood sugar: 100 mg/dL or higher
Having just one of these is common. Having three or more? That’s when your risk of heart disease jumps by 1.5 to 2 times, and your chance of developing type 2 diabetes goes up fivefold. The Framingham Heart Study showed this clearly - it’s not the sum of the parts, it’s the multiplication effect.
Why Belly Fat Is the Real Culprit
Not all fat is the same. Fat around your hips and thighs is mostly harmless. But fat inside your belly - the kind that wraps around your liver and organs - is toxic. This is called visceral fat, and it’s the engine behind metabolic syndrome.
Visceral fat doesn’t just sit there. It releases fatty acids and inflammatory chemicals directly into your bloodstream. These chemicals interfere with insulin signaling, making your muscles and liver resistant to insulin. The result? More sugar stays in your blood. Your pancreas works overtime. Your liver starts making more triglycerides. Your blood pressure climbs. Your HDL cholesterol drops.
It’s a self-sustaining cycle. The more visceral fat you have, the worse your insulin resistance gets. The worse your insulin resistance, the more fat your body stores - especially in your belly. And once this cycle starts, it doesn’t stop unless you break it.
Who’s Most at Risk?
Metabolic syndrome isn’t random. It’s tied to lifestyle, age, and genetics - but not equally for everyone.
According to CDC data from 2011-2016:
- 34.7% of U.S. adults have it
- 47% of people over 60 have it
- 38.6% of Hispanic adults are affected
- 34.2% of non-Hispanic white adults
- 31.8% of non-Hispanic Black adults
- 23.5% of non-Hispanic Asian adults
Age is a big factor. The older you get, the more your metabolism slows and your muscle mass declines - making it easier to gain belly fat. But it’s not just older people. Rates among adults aged 20-39 have jumped from 20% to nearly 30% in the last two decades.
People with polycystic ovary syndrome (PCOS) are especially vulnerable. Their hormonal imbalance makes insulin resistance worse, and many struggle to lose weight even with strict diets. That’s why metabolic syndrome is now considered the leading preventable cause of type 2 diabetes - responsible for 75 to 80% of new cases.

Why Doctors Miss It
Here’s the problem: most doctors don’t look for metabolic syndrome as a whole. They treat each piece separately.
You go in with high blood pressure. Your doctor gives you a pill. You come back with high cholesterol. They add another pill. Your fasting glucose is up? They mention prediabetes. But no one connects the dots.
On HealthUnlocked, 68% of users said their metabolic syndrome went undiagnosed - even though they had multiple risk factors. Reddit users in r/MetabolicSyndrome report the same thing: 59% feel stuck in a fragmented healthcare system where cardiologists, endocrinologists, and primary care docs treat symptoms in silos.
The truth? You don’t need five different specialists. You need one clear plan that addresses the root cause: insulin resistance.
The Only Proven Treatment: Lifestyle, Not Pills
There’s no drug approved specifically to treat metabolic syndrome. Why? Because drugs can’t fix a broken lifestyle. The only treatment that’s been proven to reverse it is a change in how you eat, move, and live.
The Diabetes Prevention Program (DPP) - a 15-year study funded by the NIH - showed that people who lost just 7% of their body weight and exercised 150 minutes a week reduced their risk of developing type 2 diabetes by 58%. That same group saw metabolic syndrome resolve in 41% of cases over 10 years.
What worked?
- Reducing daily calories to 1,200-1,500 for women, 1,500-1,800 for men
- Keeping fat intake under 25% of total calories
- Walking, cycling, or swimming 30 minutes a day, five days a week
- Cutting out sugary drinks and ultra-processed foods
It’s not about being perfect. It’s about consistency. One Reddit user lost 11% of his body weight in six months and saw his triglycerides drop from 280 to 120, his blood pressure normalize, and his fasting glucose fall below 90.

New Tools Are Making It Easier
Technology is now helping people stick to lifestyle changes.
In January 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. In a clinical trial, users who tracked their glucose and received daily coaching lost 3.2 cm off their waist and lowered their HbA1c by 0.6% in just six months - without medication.
Community health workers are also making a difference. In CDC-run programs, lay educators helped Hispanic participants lose 5.7% of their body weight - better than standard care. These programs work because they’re personal, practical, and culturally relevant.
Even insurance is starting to catch up. UnitedHealthcare reports a 22% drop in hospital visits among members in their metabolic syndrome program - saving $3,200 per person annually.
Can You Reverse It?
Yes. And not just slow it down - reverse it.
The DiRECT trial in the UK followed people with type 2 diabetes and metabolic syndrome who lost 15 kg or more through a structured, low-calorie diet. After one year, 46% of them were in full remission - no diabetes meds, normal blood sugar, and no metabolic syndrome.
That’s not a miracle. That’s biology. When you remove the excess fat - especially from your liver and pancreas - those organs start working again. Insulin sensitivity improves. Blood pressure drops. Cholesterol fixes itself.
It’s not easy. But it’s possible. And the earlier you start, the better your odds.
What to Do Next
If you’re over 40, carry extra weight around your middle, or have any two of the five risk factors, get checked. Ask your doctor for:
- A waist measurement
- A fasting lipid panel
- A fasting glucose test
- Home blood pressure monitoring over a week
If you’re diagnosed, don’t panic. Don’t wait for a pill. Start with:
- Walk 20 minutes a day - every day. No exceptions.
- Swap soda and juice for water, tea, or sparkling water.
- Replace white bread, pasta, and rice with vegetables, beans, and whole grains.
- Get 7-8 hours of sleep. Poor sleep worsens insulin resistance.
- Track your progress. Use a simple app or notebook. Weight, waist, energy levels.
You don’t need to overhaul your life overnight. Just make one change. Then another. Over time, your body will respond. Your heart will thank you.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not high enough for a diabetes diagnosis. Metabolic syndrome includes prediabetes as one of five possible components - but you can have metabolic syndrome without prediabetes, and vice versa. The key difference is that metabolic syndrome includes abdominal obesity, high blood pressure, and bad cholesterol - all of which raise your heart disease risk independently.
Can I have metabolic syndrome and still be at a normal weight?
Yes - but it’s rare. Some people, especially those with genetic conditions or severe insulin resistance, can have high visceral fat even if their overall weight looks normal. This is called "TOFI" - thin on the outside, fat inside. Waist measurement is more important than BMI. If your waist is over 35 inches (women) or 40 inches (men), you could still have metabolic syndrome even if your BMI is in the "normal" range.
Do I need medication for metabolic syndrome?
Not to treat the syndrome itself - but you may need medication for individual components. For example, if your blood pressure is dangerously high, you’ll need a blood pressure pill. If your cholesterol is very high, statins might be recommended. But drugs don’t fix insulin resistance. Lifestyle change does. Medication should support, not replace, healthy habits.
How long does it take to reverse metabolic syndrome?
Many people see improvements in just 3-6 months. Losing 5-7% of your body weight can bring blood pressure, triglycerides, and blood sugar down significantly. Full remission - where all five risk factors return to normal - usually takes 6-12 months of consistent effort. The key is sticking with it. The longer you maintain the changes, the more likely the syndrome stays gone.
Does stress cause metabolic syndrome?
Stress doesn’t directly cause it, but it makes it worse. Chronic stress raises cortisol, a hormone that increases belly fat storage and insulin resistance. It also leads to emotional eating, poor sleep, and less exercise - all of which fuel the syndrome. Managing stress through sleep, mindfulness, or movement is part of the solution.
Can children get metabolic syndrome?
Yes - and it’s rising fast. About 1 in 10 obese children in the U.S. now show signs of metabolic syndrome. The same five criteria apply, adjusted for age and sex. Early intervention - better diet, more activity, less screen time - can prevent lifelong heart disease and diabetes. Parents play a critical role in setting healthy habits.
Steve Hesketh
January 19, 2026 AT 20:23Man, I read this and felt seen. I was diagnosed last year with all five markers - belly fat, high triglycerides, low HDL, high BP, and fasting glucose at 112. Thought I was just ‘getting older.’ Turns out I was slowly killing myself with takeout and Netflix marathons. Started walking 20 mins a day, swapped soda for sparkling water, and cut out white bread. Six months later? Triglycerides down to 98, BP normal, glucose at 87. No meds. Just consistency. You don’t need a miracle. You just need to show up.
It’s not about perfection. It’s about showing up even when you’re tired. Even when you crave pizza. Even when you think it’s too late. You’re not too late. You’re right on time.
shubham rathee
January 21, 2026 AT 08:13Melanie Pearson
January 22, 2026 AT 03:53While the article presents a compelling narrative, it fails to account for the structural socioeconomic disparities that underpin metabolic syndrome in marginalized communities. The suggestion that ‘lifestyle change’ is universally accessible ignores the reality of food deserts, multi-generational poverty, and lack of paid sick leave. The DPP study cohort was largely middle-class and educated. To imply that anyone can reverse this condition with a walk and some vegetables is not just naive - it’s dangerously classist.
Barbara Mahone
January 23, 2026 AT 15:04I’m 58, diagnosed 4 years ago. Lost 32 lbs over 10 months. No keto, no fasting, no supplements. Just: no more soda, walk after dinner, sleep 7 hours, and stop eating while watching TV. My doc was shocked. Said I ‘beat the odds.’ But honestly? It wasn’t hard. It was just boring. The hardest part was not hearing ‘you’re gonna die’ every time I went in. The real win? My grandkids don’t ask if I’m ‘still sick’ anymore.
Kelly McRainey Moore
January 25, 2026 AT 02:17Amber Lane
January 27, 2026 AT 00:44Roisin Kelly
January 28, 2026 AT 14:32Samuel Mendoza
January 29, 2026 AT 04:41Yuri Hyuga
January 30, 2026 AT 12:47Let me tell you something - this isn’t just about health. It’s about dignity. When you carry that visceral fat, you carry shame too. Not because you’re weak - but because the world treats you like you’re broken. But here’s the truth: your body isn’t broken. It’s adapting. And adaptation is survival.
Every step you take, every glass of water, every night of sleep - that’s not just medicine. That’s rebellion. Against a system that sold you convenience as comfort. Against the lie that you need to be perfect to be worthy.
So if you’re reading this and you’re tired? I see you. And I’m proud of you. You’re not failing. You’re fighting. Keep going. 🌱💪
Coral Bosley
January 31, 2026 AT 02:02They say ‘lifestyle change’ like it’s some zen retreat. Try being a single mom working two jobs, surviving on food stamps, and your kid’s school lunch is the only meal you get that’s not ramen. They hand you a pamphlet on ‘walking 150 minutes a week’ like it’s a yoga class. Meanwhile, the grocery store 3 miles away doesn’t have fresh spinach - only canned corn and Slim Jims. This isn’t a personal failure. It’s a societal failure. And nobody’s fixing it.
They want you to feel guilty. Don’t. Be angry. And then fight.
MAHENDRA MEGHWAL
February 1, 2026 AT 09:15While the scientific framework presented is largely accurate, one must acknowledge the profound influence of ancestral metabolic adaptations in populations with historical exposure to periodic famine. The thrifty genotype hypothesis suggests that insulin resistance may be an evolutionary adaptation for energy conservation, which becomes pathological in environments of caloric abundance. This perspective, while often overlooked in Western clinical paradigms, is critical in understanding the disproportionate prevalence among South Asian populations, including my own family, where visceral adiposity manifests at lower BMIs. The emphasis on waist circumference over BMI is thus not merely clinical - it is anthropological.
Kevin Narvaes
February 3, 2026 AT 08:15