When your insurance denies coverage for a brand-name medication you’ve been taking for years, it’s not just a paperwork problem-it’s a health crisis. You’re not alone. In 2022, nearly 1 in 6 prior authorization requests for specialty drugs were denied, and over 60% of those were for brand-name medications. Insurers often say it’s about cost, but the real issue is formulary changes, bureaucratic delays, and a system that favors generics-even when they don’t work for you.
Why Your Insurance Denied Your Brand-Name Drug
Insurance companies don’t deny brand-name drugs because they’re evil. They do it because their formularies are designed to push cheaper alternatives. But here’s the catch: not all generics are created equal. For some patients, switching from a brand-name drug to a generic can cause serious side effects, reduced effectiveness, or even dangerous health events. Think insulin for type 1 diabetes, seizure meds like Lamictal, or biologics for autoimmune conditions. These aren’t simple substitutions. Many denials happen because your insurer suddenly removed your medication from their formulary without telling you. Under ERISA-governed plans (which cover over 60% of working Americans), they don’t need to give you advance notice. You find out when you go to fill your prescription and the pharmacy says, “Sorry, not covered.”What You Need Before You Appeal
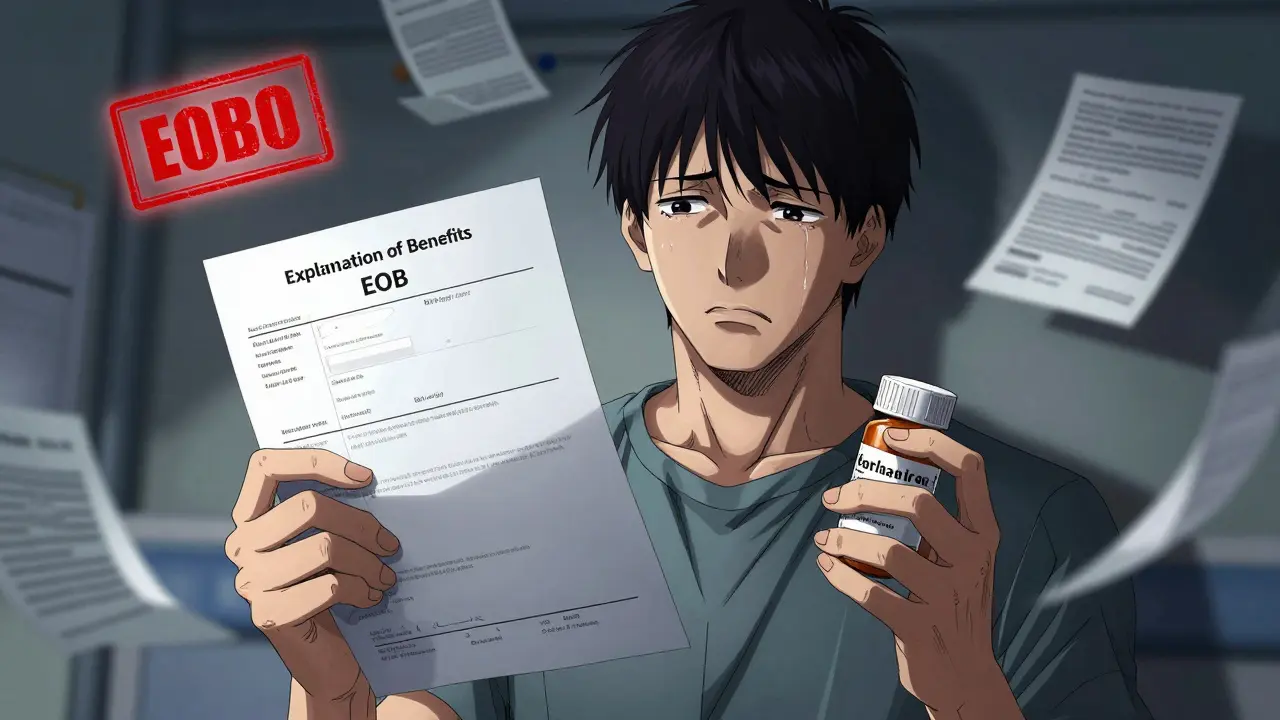
You can’t appeal without proof. The first step is getting your Explanation of Benefits (EOB) document. By law, your insurer must send this within 5 business days of denying your claim. Read it carefully. It will list the exact reason: “generic alternative available,” “prior authorization not approved,” or “not medically necessary.” Write that reason down. You’ll need it. Next, call your doctor’s office. Ask them to write a letter of medical necessity. This isn’t a form letter. It needs to be detailed. Your doctor must include:- Your diagnosis and how the brand-name drug treats it
- Specific examples of when generic versions failed you-like hospital visits, side effects, or loss of symptom control
- Lab results, dosage history, and any previous prior authorization numbers
- Why switching would harm your health, not help it
The Two-Stage Appeal Process
There are two stages to fighting a denial: internal and external review. Stage 1: Internal AppealThis is your first shot. You submit your letter, EOB, and any supporting documents directly to your insurer. You have 180 days from the denial date to file under most plans (120 days for Medicare). For urgent cases-like if you’re running out of insulin or your condition is worsening-you can request an expedited review. Insurers must respond within 4 business days in those cases. Don’t just mail it and wait. Call the insurance company every other day. Ask for the name of the person handling your case. Get a reference number. Document every call. Kantor & Kantor’s data shows appeals with consistent follow-up are processed 28% faster. Stage 2: External Review
If your internal appeal gets denied, you move to the external review. This is where things change. An independent third party-approved by the government-reviews your case. No one from your insurance company is involved. This stage has a much higher success rate: 58% compared to just 39% for internal appeals. For non-ERISA plans (like Medicaid or individual market plans), you file with your state’s insurance commissioner. For ERISA plans (most employer-based coverage), you file with the U.S. Department of Health and Human Services. The process takes 30 to 60 days. But here’s the kicker: if you’ve got strong clinical documentation, your odds jump to 68% approval, according to the Bleeding Disorders Advocacy Alliance.
When to Bring in a Lawyer
Most people think they can handle this alone. And they can-sometimes. But if your case involves an ERISA plan, you’re playing on a field stacked against you. Insurance companies have teams of lawyers who know every loophole. A 2023 study by Kantor & Kantor found that appeals drafted by attorneys were 47% more likely to succeed than those filed by patients themselves. You don’t need a lawsuit yet. But if your internal appeal is denied and you’re facing a life-altering medication loss-like a biologic for Crohn’s disease or a specialty drug for multiple sclerosis-hire a lawyer who specializes in ERISA and health insurance denials. They’ll know how to frame your case to bypass the insurer’s legal traps.Real Stories: What Works
One Reddit user, ‘DiabeticDad87,’ got his child’s Humalog insulin denied. He didn’t argue about cost. He sent his doctor’s letter showing three hospitalizations from hypoglycemia after switching to a cheaper insulin. Approval came in 11 days. Another patient, ‘ChronicPainPatient’ on PatientsLikeMe, fought a 6-month battle over a brand-name migraine drug. The insurer kept saying, “Try a generic.” But the generic didn’t touch her symptoms. She finally hired a lawyer. The appeal won-but cost $2,500. She said it was worth every penny. A 2022 survey by the Patient Advocate Foundation found that 61% of people felt overwhelmed by the process. And 44% said they couldn’t have won without help from their doctor or a legal advocate.
What to Do While You Wait
Appeals take time. You can’t stop your medication. So what do you do now? Many drugmakers offer patient assistance programs. Eli Lilly’s Insulin Value Program, for example, gives brand-name insulin for $35 a month to anyone without full coverage. Other companies like AbbVie, Amgen, and Roche have similar programs. Go to their websites and search for “patient assistance” or “copay card.” Some pharmacies will give you a 30-day supply while your appeal is pending. Ask your pharmacist. They often have connections with drug manufacturers. And if you’re on Medicare Part D, use the real-time benefit tool before you fill any prescription. Since 2023, all Part D plans are required to show you coverage status upfront. That way, you won’t get denied at the counter.The Bigger Picture
The system is broken. In 2023, 56% of commercial plans required prior authorization for more than half of brand-name specialty drugs-up from 38% just five years ago. Doctors now spend over 13 hours a week just managing these denials. But change is coming. The Biden administration’s 2023 executive order pushed CMS to enforce appeal rights harder. The proposed Improving Seniors’ Timely Access to Care Act could cut approval delays for Medicare patients by half. And AI tools are starting to flag inappropriate denials before they happen. For now, though, you have to fight. And you can win. Not every denial deserves an appeal-some are just bad prescribing. But if your doctor says the brand-name drug is medically necessary, and you’ve tried everything else, then you have every right to demand coverage.What if my insurance says a generic is just as good?
Insurers often assume generics work the same for everyone. But for many medications-especially biologics, anticonvulsants, and psychiatric drugs-small differences in formulation can cause big changes in how your body responds. Your doctor’s letter must prove this with specific examples: side effects, failed attempts, lab results, or hospitalizations tied to the generic switch.
How long do I have to file an appeal?
Most private insurance plans give you 180 days from the denial date. Medicare gives you 120 days. Medicaid varies by state-check your state’s rules. For urgent cases, you can request an expedited review, which requires a decision within 4 business days. Don’t wait. Delays reduce your chances.
Can I appeal if I’m on Medicare or Medicaid?
Yes. Medicare Part D and Medicaid both have formal appeal processes. Medicare uses a five-level system, starting with a redetermination request. Medicaid appeals go through your state’s Medicaid agency. The rules are different, but your rights are the same: you can challenge denials based on medical necessity.
Do I need to pay for the medication while waiting?
You shouldn’t have to. Many drug manufacturers offer temporary free or low-cost supplies while your appeal is pending. Ask your pharmacist or visit the manufacturer’s website. Some pharmacies will also give you a 30-day bridge supply. Don’t go without your medication-there are options.
What if my appeal is denied twice?
If you’ve been denied internally and externally, you can file a complaint with your state insurance commissioner or the U.S. Department of Health and Human Services. For ERISA plans, you may also have the right to sue-but only after exhausting all appeals. At that point, hiring a lawyer is critical. Federal courts don’t allow juries in ERISA cases, so your case must be airtight.
Can my doctor help me with the appeal?
Absolutely. In fact, 78% of successful appeals involve active participation from the prescribing physician. Ask them to write a detailed letter of medical necessity, call the insurer on your behalf, or even submit a peer-to-peer review request. Many insurers will speak directly with your doctor if you request it.
Jason Shriner
January 11, 2026 AT 19:42Jennifer Littler
January 12, 2026 AT 09:00Vincent Clarizio
January 12, 2026 AT 20:24Adewumi Gbotemi
January 14, 2026 AT 11:02Matthew Miller
January 14, 2026 AT 21:44Alfred Schmidt
January 16, 2026 AT 10:39Priscilla Kraft
January 17, 2026 AT 20:46Christian Basel
January 19, 2026 AT 20:20Alex Smith
January 19, 2026 AT 22:34Roshan Joy
January 20, 2026 AT 12:06Michael Patterson
January 21, 2026 AT 07:18Madhav Malhotra
January 22, 2026 AT 19:47Priya Patel
January 23, 2026 AT 00:31Sean Feng
January 24, 2026 AT 00:02