One wrong dose. One misread label. One skipped step. That’s all it takes for a routine medication to turn deadly. In hospitals and clinics across the country, staff are required to perform extra verification procedures on a short list of medications that can kill if handled incorrectly. These aren’t just routine pills - they’re high-risk drugs where even a small mistake leads to cardiac arrest, organ failure, or death. And yet, despite years of guidelines, many of these safety steps are being skipped - not because staff are careless, but because the system is broken.
What Makes a Medication High-Risk?
Not all medications are created equal. A typo on a prescription for ibuprofen might cause a stomach ache. A typo on a prescription for IV insulin? It can drop a patient’s blood sugar to zero in minutes. That’s why the Institute for Safe Medication Practices (ISMP) defines high-alert medications as those with a heightened risk of causing significant harm when used in error. These drugs don’t just cause side effects - they cause irreversible damage if the dose is off by even 10%. The most common high-risk medications requiring extra verification include:- Insulin (all forms - especially IV and concentrated solutions)
- IV opioids like morphine, fentanyl, and hydromorphone
- Heparin (both intravenous and subcutaneous)
- Chemotherapy agents (antineoplastic drugs)
- Potassium chloride concentrate
- Cardiovascular drugs like sodium nitroprusside, epinephrine, and vasopressin
The Double Check: How It’s Supposed to Work
The standard safety protocol is called an independent double check. It’s not two people glancing at the same label. It’s two qualified professionals - usually a nurse and a pharmacist - verifying every detail separately, without seeing each other’s work. The goal is to catch mistakes that one person might miss. Here’s what they check, step by step:- Right patient - Two identifiers, like name and date of birth, verified against the wristband and order.
- Right drug - The name, strength, and form must match the prescription exactly. Confusing “morphine” with “hydromorphone” is a common error.
- Right dose - Calculations are re-done manually. A nurse might calculate a dose based on weight, then the pharmacist re-calculates it independently.
- Right route - IV vs. oral vs. epidural. Giving insulin subcutaneously instead of IV can be fatal.
- Right time - Is this dose due now? Was the last one given on schedule?
- Right documentation - Both providers sign the electronic MAR (Medication Administration Record) after verification.
- Right reason - Is this drug still needed? Has the patient’s condition changed?
- Right response - What side effects should we watch for?
- Right to refuse - Has the patient been informed and given the chance to say no?
Where the System Fails
You’d think this system is bulletproof. But in real hospitals, it’s not. A 2022 ISMP survey found that 68% of nurses admitted skipping required double checks during busy shifts. Why? Forty-two percent said there simply wasn’t a second person available. Others said it took too long. Some said they’d done the same check a hundred times before - “I know what I’m doing.” That’s the dangerous myth. Human memory is fallible. Fatigue clouds judgment. A nurse who’s worked 12 hours straight might see “10 units” and assume it’s correct, even if the order says “100 units.” That’s exactly how patients die. Another problem: confirmation bias. If the first nurse checks the dose and says “Looks good,” the second nurse often just nods along. That’s not independent verification. That’s groupthink. True double checks require the second person to do their own math, their own lookup, their own visual inspection - without being influenced. And in community hospitals, staffing shortages make this nearly impossible. One nurse is managing five patients. The pharmacist is in the back filling 20 orders. Who has time to stop and double-check every insulin dose?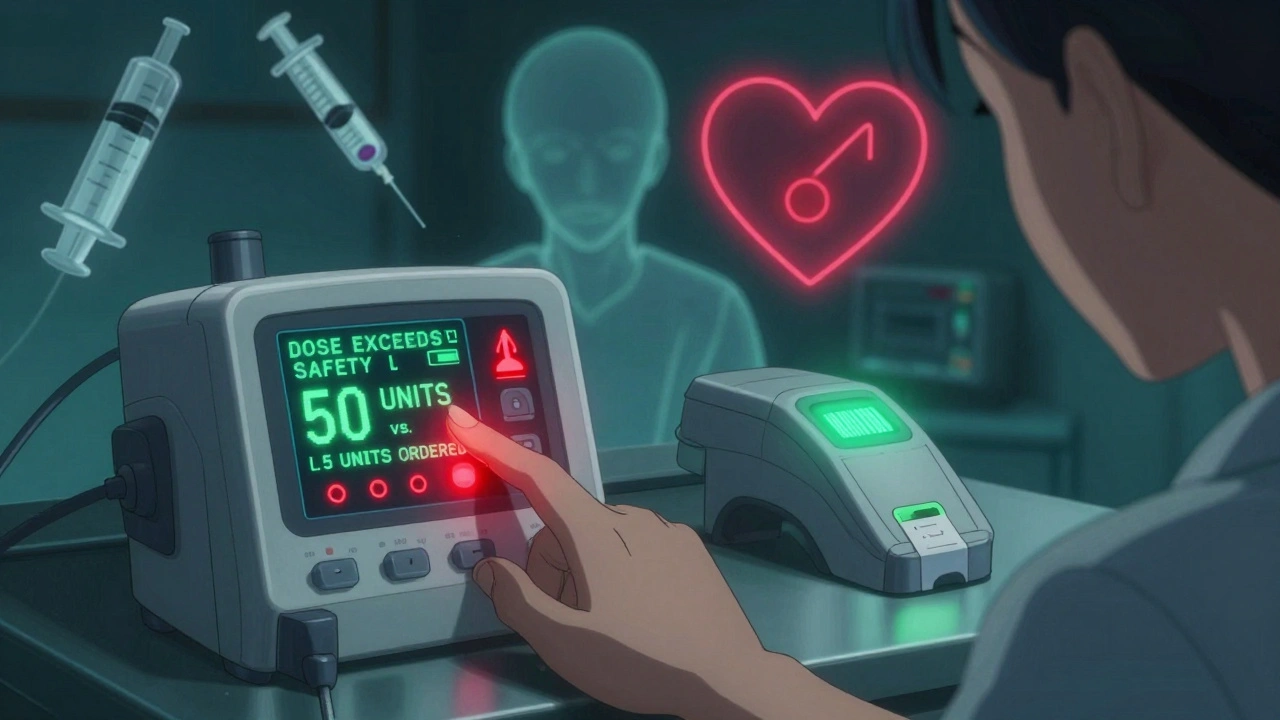
Technology Is Changing the Game
The solution isn’t just more people. It’s smarter systems. Barcode scanning at the bedside is now the gold standard for catching the wrong drug or wrong patient. When a nurse scans the patient’s wristband and the medication label, the system instantly compares them to the electronic order. If there’s a mismatch - say, the drug is right but the dose is wrong - the system alarms. No human error. No skipped step. For infusion pumps, smart technology can now prevent dangerous dosing. A pump programmed for insulin will only accept doses within safe limits. If someone tries to set 50 units instead of 5, the pump refuses to run. The Department of Veterans Affairs (VHA) is leading the way. By 2024, all VA facilities will use barcode scanning for high-risk meds, with manual double checks reserved only for complex cases - like preparing custom chemotherapy bags or adjusting high-dose heparin infusions. This isn’t about cutting corners. It’s about focusing human effort where it matters most.What’s Changing Now - And What You Should Know
The old rule - “double check everything” - is being replaced with a smarter one: “double check only what matters.” The ISMP now advises hospitals to focus verification efforts on just four high-risk scenarios:- IV opioids
- IV insulin
- IV heparin
- IV chemotherapy

What Patients Can Do
You don’t have to be a nurse to help prevent errors. If you or a loved one is receiving one of these high-risk medications, ask:- “Is this the right drug and dose?”
- “Can I see the label before it’s given?”
- “Are two people checking this?”
The Bottom Line
High-risk medications aren’t the enemy. They’re lifesavers when used correctly. But they’re also weapons in the wrong hands. The goal isn’t to make staff do more paperwork - it’s to make sure the right person gets the right drug, at the right time, in the right way. Technology helps. Better training helps. But the most powerful tool is awareness. If you work in healthcare, don’t skip the check. If you’re a patient, don’t stay silent. One extra step - done right - can mean the difference between life and death.What medications require a double check in hospitals?
Medications that require independent double checks include IV insulin, IV opioids like morphine and fentanyl, IV heparin, chemotherapy drugs, and concentrated potassium chloride. These are listed as high-alert medications by the Institute for Safe Medication Practices (ISMP) because even small errors can cause death. Some hospitals also require double checks for other cardiovascular drugs, TPN, and pediatric cardiac medications.
Who can perform a double check?
Only qualified healthcare professionals can perform double checks. This typically includes registered nurses, pharmacists, and prescribers like doctors or nurse practitioners. In some settings, physician assistants may also be authorized. The second person must be independent - meaning they verify the medication without seeing the first person’s work to avoid bias.
Is a double check always necessary?
No. Current guidelines from the ISMP recommend focusing double checks on the highest-risk medications - like IV insulin, IV opioids, and chemotherapy - rather than requiring them for every drug. Overusing double checks leads to fatigue and workarounds. Technology like barcode scanning now handles many routine verifications more reliably than manual checks.
What happens if a double check is skipped?
Skipping a double check increases the risk of a medication error, which can lead to serious harm or death. Hospitals track these incidents as safety events. Repeatedly skipping checks can result in mandatory retraining, disciplinary action, or even loss of licensure. More importantly, it puts patients at unnecessary risk. Even one skipped step can be fatal with high-alert medications.
Can patients ask if a double check was done?
Yes. Patients and families are encouraged to ask questions about their medications. Simple questions like, “Is this the right drug?” or “Are two people checking this?” can help catch errors. Many hospitals now train staff to welcome this kind of involvement - it’s part of a safety culture where everyone, including patients, plays a role in preventing mistakes.

Ignacio Pacheco
December 2, 2025 AT 22:09So let me get this straight - we’re still relying on humans to catch errors in high-risk meds, when a barcode scanner and a smart pump could do it in 0.2 seconds? The system isn’t broken - it’s just stubborn.
Jim Schultz
December 4, 2025 AT 01:43Oh, absolutely - and let’s not pretend that ‘double-checking’ is anything more than performative theater! I’ve seen nurses glance at a label, nod, and move on - while the pharmacist is 12 charts deep in EHR chaos. The real problem? We treat safety like a checklist, not a culture. And no - ‘I’ve done this a hundred times’ is not a valid clinical rationale. It’s a death sentence waiting for a typo.
Barcodes? Smart pumps? Of course they work. But hospitals still cling to the myth that ‘human vigilance’ is the gold standard - as if fatigue, burnout, and 14-hour shifts don’t exist. The VA’s model is the only sane approach: automate the routine, reserve human judgment for the complex. Why? Because humans are terrible at repetition. Machines aren’t.
And don’t get me started on the ‘independent’ double-check. Independent? Ha. The second nurse sees the first one’s signature and just ticks the box. Confirmation bias is alive, well, and killing patients. You want real safety? Eliminate the illusion of human infallibility. Period.
Also - why are we still using paper MARs in 2024? And why is potassium chloride still labeled like a grocery item? I’ve seen vials that look like juice boxes. Someone’s gonna die because a nurse thought it was apple cider. It’s not negligence - it’s design failure.
And yes - patients should ask questions. But shouldn’t the system be designed so they don’t have to? We’ve outsourced safety to the patient because we’re too lazy to fix the infrastructure. That’s not empowerment - that’s abandonment with a smiley face.
Stop glorifying ‘double-checks.’ Start investing in systems that don’t rely on tired, overworked people to be perfect. Because they won’t be. And people will die. Again.
Katherine Gianelli
December 5, 2025 AT 03:24I’ve worked in the NICU for 17 years and I can tell you - every time we double-check a cardiac med, I feel like I’m holding a baby’s heartbeat in my hands. It’s not just procedure - it’s love in action. I’ve seen kids bounce back because someone paused, looked again, and caught a decimal point that was off by one. That’s the quiet heroism no one talks about.
But you’re right - it shouldn’t be on us to be perfect. We need better tools, better staffing, better training. Not just more checkboxes. We need to feel supported, not just monitored.
If you’re a nurse reading this - you’re doing important work. Even on the hardest days. Keep going. And if you’re a patient - thank you for asking questions. That matters more than you know.
Makenzie Keely
December 5, 2025 AT 10:26Let’s be crystal clear: skipping a double check on IV insulin isn’t a ‘mistake’ - it’s a criminal act of negligence. The fact that 68% of nurses admit to skipping them? That’s not a system failure - that’s a moral failure. And the hospitals that allow it? They’re complicit.
Barcodes help. Smart pumps help. But if your hospital still lets nurses bypass safety protocols because they’re ‘busy,’ then your hospital has chosen profit over patients. And that’s not healthcare - that’s a death sentence with a clipboard.
Patients: demand to see the label. Demand to know who verified it. Demand that your nurse stop rushing. Your life is not a speedrun.
Vincent Soldja
December 6, 2025 AT 00:00Double checks are inefficient. Automation is better. End of story.
Kidar Saleh
December 6, 2025 AT 23:53In the UK, we’ve adopted a similar framework - but with one key difference: we call it ‘safety culture,’ not ‘compliance.’ It’s not about ticking boxes - it’s about creating an environment where speaking up is rewarded, not punished. I’ve seen junior nurses stop a senior nurse from administering a wrong dose - and instead of being reprimanded, they were given a plaque. That’s the kind of culture that saves lives.
Technology helps. But people - truly supported, respected people - are the real safety net.
Joykrishna Banerjee
December 7, 2025 AT 03:41Look, let’s be honest - most of these nurses are underqualified, overworked, and underpaid. But that doesn’t excuse the fact that they’re still using analog systems in a digital age. The real issue? The entire medical-industrial complex is built on exploitation. You think they care about your life? They care about billing codes. Double checks are a Band-Aid on a hemorrhage.
And don’t even get me started on ‘patient involvement.’ You think a diabetic grandma is going to understand the difference between concentrated and regular insulin? Please. This is performative safety for the boardroom. Real safety requires systemic overhaul - not patient empowerment theater.
Also, why are we still using ‘heparin’ and not ‘LMWH’? Terminology is a gateway to error. Someone should’ve fixed this 20 years ago.
Chloe Madison
December 8, 2025 AT 22:46As a nurse educator, I train new staff on high-alert meds every week - and I always start with this: ‘If you’re rushing, you’re already wrong.’
We don’t need more rules. We need more time. More staff. More respect. When you treat nurses like replaceable cogs, you get cogs that skip steps. But when you treat them like the experts they are - they rise to the occasion.
And yes - patients, please ask questions. You’re not being annoying. You’re being brave. And we need more of you.
Also - if your hospital still uses handwritten orders for insulin? Run. Find another one.
Francine Phillips
December 9, 2025 AT 06:19My dad got the wrong dose of heparin once. He lived. But I still don’t trust hospitals.
parth pandya
December 10, 2025 AT 18:40in india we dont have enough nurses for double check so we use barcode scanner and smart pump only. its work good. no one die. so why usa still do manual check?
Myson Jones
December 11, 2025 AT 22:37I appreciate the intent behind this piece - and I agree with the shift toward targeted verification. But I’d urge hospitals to consider the psychological burden of constant vigilance. When safety becomes a ritual rather than a shared value, it loses its meaning. The goal isn’t just to prevent errors - it’s to preserve the humanity of care.