HCC surveillance isn’t just a good idea-it’s a lifesaver. Hepatocellular carcinoma (HCC) is the most common type of liver cancer, causing over 800,000 deaths worldwide each year. But catch it early, and survival rates jump from under 20% to over 70%. For people with cirrhosis, regular screening is the difference between a treatable condition and a fatal diagnosis.
What is HCC and why does cirrhosis matter?
Hepatocellular Carcinoma (HCC) is a cancer that starts in the liver’s main cells. It’s linked to chronic liver damage, especially cirrhosis, where scar tissue replaces healthy liver tissue. About 80% of HCC cases happen in people with cirrhosis. The World Health Organization reports over 900,000 new HCC cases annually. Without early detection, HCC often spreads before symptoms appear, making treatment harder.
How HCC surveillance works
Surveillance means regular checks for HCC in high-risk people. For cirrhosis patients, this usually means an ultrasound every six months. Why? HCC tumors typically grow 1-2 cm in that time frame. If caught early, treatments like surgery or ablation can remove them completely. Studies show surveillance improves 5-year survival from 10-20% to 50-70%. The American Association for the Study of Liver Diseases (AASLD) strongly recommends this for all adults with Child-Turcotte-Pugh (CTP) Class A or B cirrhosis. Some guidelines also suggest adding alpha-fetoprotein (AFP) blood tests, but this is less certain. An AFP level above 20 ng/mL usually triggers further imaging.
| Guideline | Surveillance Interval | AFP Testing | Risk Stratification | Notes |
|---|---|---|---|---|
| AASLD 2018 | Biannual ultrasound | Conditional (threshold >20 ng/mL) | No risk stratification | Strong recommendation for Child-Pugh A/B cirrhosis |
| EASL 2023 | 6-month ultrasound (risk-based) | Not routinely recommended | High (≥2.5%), Medium (1.5-2.5%), Low (<1.5%) | Targets highest-risk patients; may reduce unnecessary tests |
| APASL 2017 | Biannual ultrasound | Recommended with ultrasound | Some risk factors considered | Surveillance for some Child-Pugh C patients |

Why real-world implementation falls short
Despite clear guidelines, many patients miss out on surveillance. In the U.S., only 41.7% of cirrhotic patients diagnosed with HCC had prior screening. Black patients (34.1%) and Medicaid recipients (31.6%) face bigger gaps than White patients (52.3%) or privately insured people (48.2%). Primary care doctors often don’t know when to refer patients for screening. A VA report found only 30-50% of eligible cirrhotic patients get proper surveillance. Electronic health record reminders could fix this-studies show they boost adherence from 35% to 68%. Patient navigators also help, cutting missed appointments from 32% to 14%.
Treatment options depend on stage
Early-stage HCC (Barcelona Clinic Liver Cancer stage 0 or A) is curable. Options include:
- Liver transplant: Removes the cancer and damaged liver. Best for patients with small tumors and severe cirrhosis.
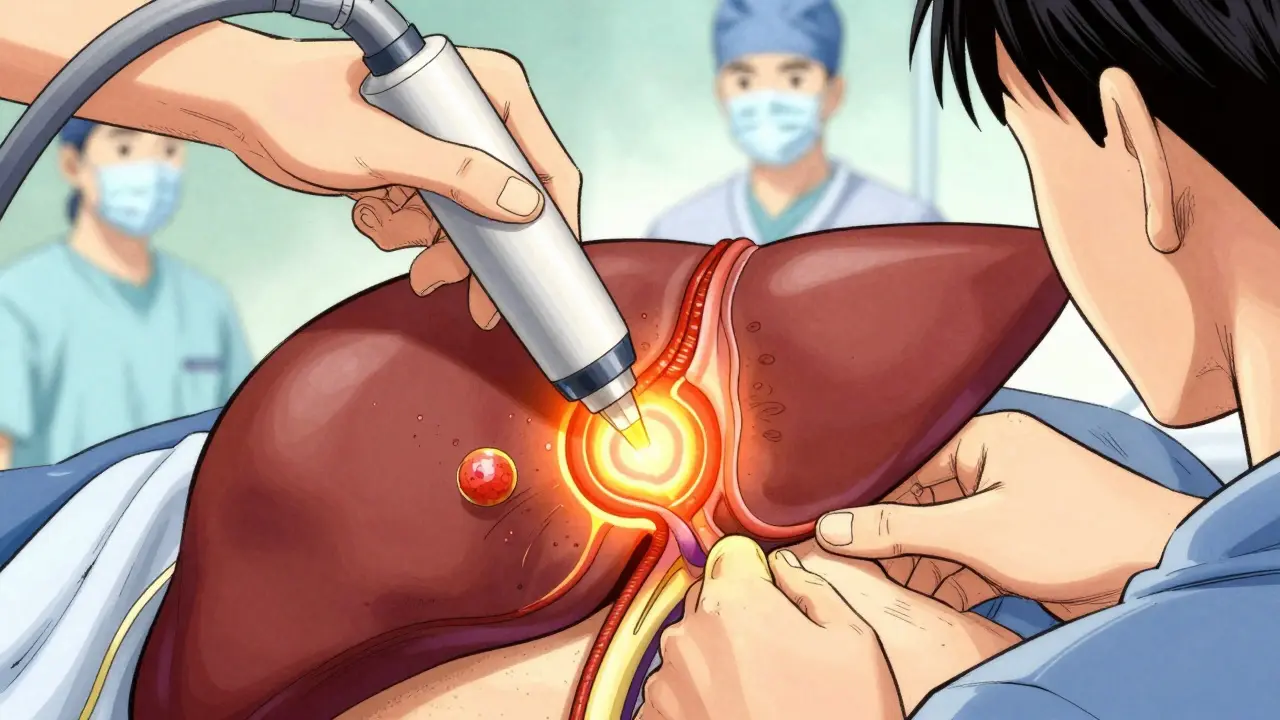
- Radiofrequency ablation: Uses heat to destroy tumors under 3 cm. No major surgery needed.
- Surgical resection: Removes the tumor portion of the liver. Requires good liver function.
Advanced HCC (stage B or later) uses systemic drugs like sorafenib or lenvatinib. These slow tumor growth but don’t cure the cancer. The key is catching HCC early-70% of screen-detected tumors are early-stage, versus 30% in unscreened cases. This is why surveillance matters.
What’s next for HCC detection
New tools are making surveillance smarter. The FDA-approved Medtronic LiverAssist AI tool boosts ultrasound accuracy by 18-22% for small tumors. The GALAD score (gender, age, AFP-L3, AFP, DCP) detects early HCC with 85% sensitivity. The SURVIVE study, tracking 10,000 cirrhotic patients, will release results in late 2025 to test risk-based surveillance. By 2027, abbreviated MRI scans (5-7 minutes) might replace ultrasound for high-risk patients. Costs are dropping too-$350-400 per scan versus $500+ historically.
What patients can do today
If you have cirrhosis, ask your doctor about HCC surveillance. Don’t skip ultrasounds-even if you feel fine. Early HCC rarely causes symptoms. Keep track of appointments: patient navigators can help if you miss check-ups. If your AFP is elevated, get follow-up imaging immediately. Most importantly, manage your cirrhosis. Avoid alcohol, control hepatitis B/C, and maintain a healthy weight. These steps lower your HCC risk and make surveillance more effective.
What is HCC surveillance?
HCC surveillance is regular monitoring for liver cancer in people with cirrhosis. It typically involves ultrasound scans every six months and sometimes blood tests like AFP. The goal is to find tumors early when they’re small and treatable, improving survival chances dramatically.
How often should I get screened for HCC if I have cirrhosis?
Most guidelines recommend ultrasound every six months. The AASLD and EASL both support this for adults with Child-Pugh Class A or B cirrhosis. Some risk-based models adjust this frequency based on individual factors like hepatitis status or liver function.
What happens if my ultrasound shows a liver mass?
A mass larger than 1 cm on ultrasound requires immediate follow-up with contrast-enhanced CT or MRI. This helps confirm if it’s HCC. The Liver Imaging Reporting and Data System (LI-RADS) standardizes how radiologists interpret these scans, improving accuracy. If confirmed, your care team will discuss treatment options based on the tumor’s size and stage.
Is AFP testing necessary for HCC surveillance?
Not always. The AASLD conditionally recommends AFP testing (threshold >20 ng/mL), but evidence is low-quality. EASL doesn’t routinely include it. AFP can miss early HCC or give false positives from other liver conditions. Ultrasound alone is often sufficient for surveillance, especially when combined with risk stratification.
Can I skip surveillance if I feel fine?
No. Early HCC rarely causes symptoms. Many patients feel perfectly healthy until the cancer is advanced. Skipping surveillance means missing the chance for curative treatment. Even if you’re asymptomatic, stick to your screening schedule-it’s the best way to catch HCC early.
Mary Carroll Allen
February 7, 2026 AT 02:53Wow, this is such an important topic! I've been living with cirrhosis for a few years now, and I can't believe how many people don't know about regular HCC surveillence. The stats are stagering-catching it early can boost survival from under 20% to over 70%!
I always thought it was just a routine checkup, but it's literally the difference between life and death.
My doc told me to stay on top of it, and I've been sticking to it religiously.
It's crazy how many people skip screenings because they feel fine, but early HCC has no symptoms. Trust me, I've been there-no symptoms until it's too late.
This needs to be shouted from the rooftops. If you have cirrhosis, don't skip those checkups. It's not just a recommendation-it's a must.
Also, the comparison table in the post is super helpful. AASLD and EASL both say ultrasound every 6 months, but EASL is more risk-based. Still, for most people, it's the same advice.
Seriously, this info could save lives. I'm going to share this with my support group. Everyone needs to know.
Joey Gianvincenzi
February 8, 2026 AT 17:53Your perspective is commendable, yet it lacks the necessary rigor. The data presented in the article is accurate, but the emphasis on surveillance must be contextualized within global healthcare disparities. In many developing nations, access to ultrasound technology is severely limited, rendering such recommendations impractical. It is imperative to address systemic inequities before advocating for universal adherence to surveillance protocols.
Amit Jain
February 8, 2026 AT 18:44Surveillance? What a joke. The whole HCC screening thing is a scam. Ultrasound every six months? That's just a way for hospitals to make money. Most people with cirrhosis don't even get cancer. They're just scaring people into unnecessary tests.
I've read studies that show AFP blood tests are more reliable, but even those aren't perfect.
It's all about profit. Big Pharma and hospitals push this stuff to keep people coming in. I'm not falling for it. If you feel fine, why get tested? You're just wasting time and money.
Sarah B
February 9, 2026 AT 19:11Screening saves lives. Period.
Eric Knobelspiesse
February 10, 2026 AT 23:35Sarah, your point is valid but oversimplified. Let's dig deeper. The psychological impact of false positives is huge-imagine the stress of a false alarm. And the costs of unnecessary biopsies or treatments.
It's not just black and white. The system is flawed. We need to question the assumptions.
Maybe surveillance isn't the solution. Maybe we need better prevention.
But hey, I'm just a guy on the internet. Take it with a grain of salt.
Typo: 'principls' not 'principles'-wait, no, that's correct. Oops.
Heather Burrows
February 11, 2026 AT 19:46I don't know. I mean, the article says surveillance is important, but I'm not sure. Maybe it's just for people who don't take care of themselves. Like, if you have cirrhosis, you probably did something to cause it. So why should we waste resources on them?
I'm just saying. Maybe they should have thought about it before drinking too much.
It's not my problem. I'm not a doctor. Just saying.
Ritu Singh
February 13, 2026 AT 10:06Your perspective is narrow and lacks empathy. Cirrhosis can result from many causes beyond lifestyle choices, including genetic and viral factors. It is our collective responsibility to support those affected, regardless of the origin of their condition. Healthcare should be equitable and compassionate. Let's focus on solutions, not judgment.
Mark Harris
February 14, 2026 AT 03:22Heather, that's not cool. People with liver issues deserve care, no matter why they got there. It's not about blame-it's about helping. Let's lift each other up, not tear each other down. We're all in this together!
Savannah Edwards
February 14, 2026 AT 15:34Ritu, I really appreciate your thoughtful response. It's so important to approach healthcare with empathy and inclusivity. Cirrhosis isn't always about personal choices-viral hepatitis, autoimmune issues, and even genetic factors play a role.
I've worked with patients from all walks of life, and their stories remind me that everyone deserves dignity and care.
Surveillance isn't about blame; it's about giving people the best chance to live.
We need to remember that behind every statistic is a human being with a family, dreams, and fears.
Let's keep the conversation compassionate and solution-focused. It's not just about medicine-it's about humanity.
Mayank Dobhal
February 14, 2026 AT 19:58Surveillance is key. Period. Get checked. Don't wait. It's that simple.
Skip it, and you're risking everything. No excuses.
Marcus Jackson
February 15, 2026 AT 00:47Yeah, but you're oversimplifying. It's not just 'get checked.' There's more to it. Like, what if you can't afford it? Or what if the test isn't accurate?
It's not as simple as you think. Just saying.