Scaly Skin Food Trigger Checker
Check if a food is commonly associated with triggering scaly skin conditions. Enter a food item and select your condition to see if it's typically problematic.
Ever wonder why a plate of pizza sometimes seems to make your skin feel tighter and more “scratch‑y”? It’s not just a coincidence-what you eat can directly affect the way scaly skin conditions behave. Below we’ll untangle the science, point out the usual suspects, and give you a practical food plan that actually works.
What Are Scaly Skin Overgrowths?
Scaly Skin Overgrowths is a group of dermatological conditions marked by thick, flaky patches that can be itchy, painful, or both. The most common members of this family include Psoriasis - an immune‑driven disease that speeds up skin cell turnover, leading to raised, silvery scales - and Keratosis pilaris, the harmless “chicken‑skin” bumps that love the upper arms and thighs.
Other players are Seborrheic dermatitis, which thrives in oily areas like the scalp, and Eczema, a condition that can swing between weepy and scaly depending on the trigger.
Why Diet Matters for Your Skin
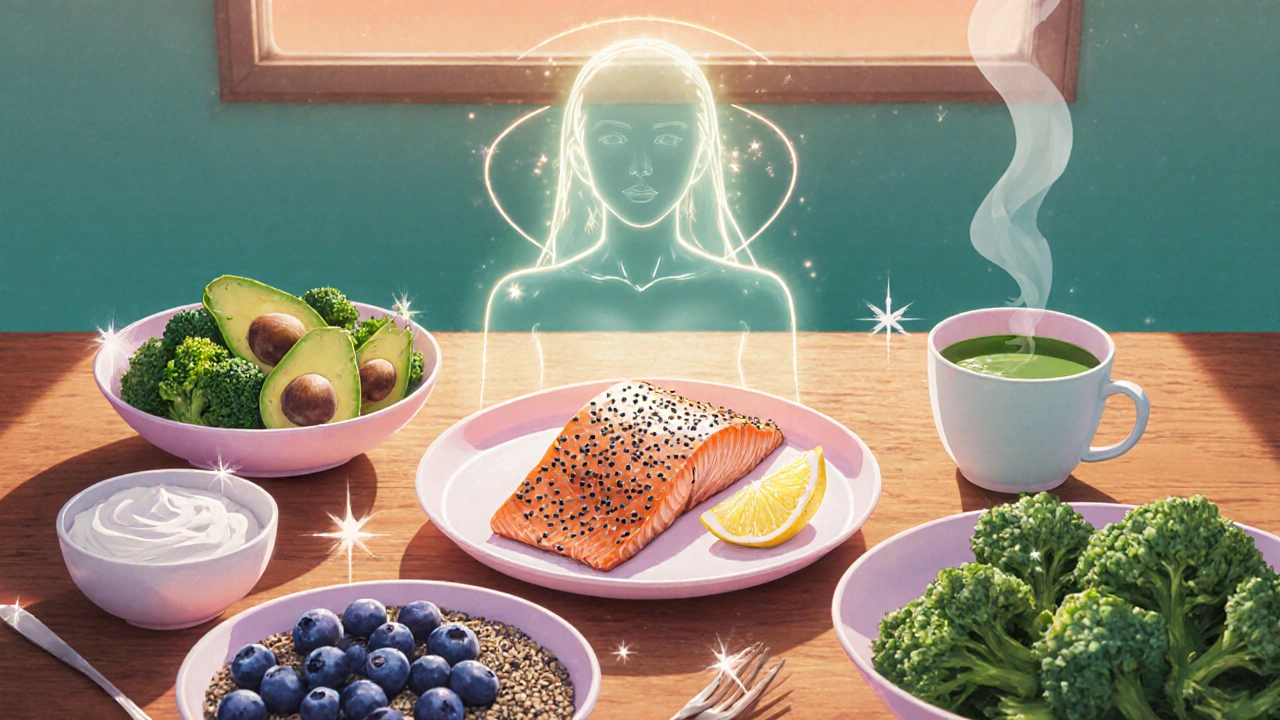
Skin isn’t a passive barrier; it’s an active organ that reflects the nutrients you feed it. When you consume foods that trigger inflammation, your immune system goes into overdrive, and that flare can show up as extra scaling or redness. Conversely, anti‑inflammatory foods calm the system, helping the skin regenerate more smoothly.
Think of it like a garden: too much fertilizer (sugar, processed fats) will cause weeds (flare‑ups), while compost (omega‑3s, antioxidants) supports healthy growth.
Key Nutrients That Keep Scaly Skin in Check
- Omega‑3 fatty acids - found in fatty fish, chia seeds, and walnuts - reduce the production of inflammatory molecules (like prostaglandins) that aggravate psoriasis.
- Vitamin D - sunlight‑derived and present in fortified dairy - helps regulate skin cell growth, which is overly rapid in many scaly conditions.
- Probiotics - from yogurt, kefir, or a quality supplement - nurture a balanced gut microbiome, which recent studies link to lower skin inflammation.
- Antioxidants (vitamins C & E, polyphenols) - present in berries, leafy greens, and green tea - protect skin cells from oxidative stress.
- Gluten - for a small subset of people with celiac disease or non‑celiac gluten sensitivity, eliminating gluten can dramatically reduce scaling.
Foods That Frequently Trigger Flare‑Ups
Not every trigger hits everyone, but research and patient reports point to a handful of common culprits:
- Refined sugar and high‑glycemic carbs - cause spikes in insulin, which can boost inflammatory pathways.
- Processed meats and saturated fats - raise levels of arachidonic acid, a precursor to pro‑inflammatory eicosanoids.
- Dairy - some people notice a direct link between cheese or whole milk and worsened scaling, especially in seborrheic dermatitis.
- Alcohol - dehydrates skin and can disrupt the gut barrier, making flare‑ups more likely.
- Nightshade vegetables (tomatoes, peppers, eggplant) - contain lectins that, for a minority, may provoke skin irritation.
Putting It All Together: A Sample Day of Skin‑Friendly Eating
Below is a simple 1,800‑calorie menu that hits the nutrients above while steering clear of the usual triggers.
- Breakfast: Greek yogurt with a tablespoon of chia seeds, fresh blueberries, and a drizzle of honey (if you tolerate sugar).
- Mid‑morning snack: A handful of almonds and an orange.
- Lunch: Grilled salmon on a mixed‑leaf salad with spinach, avocado, cucumber, and a lemon‑olive‑oil dressing.
- Afternoon snack: Carrot sticks with hummus (cumin adds anti‑inflammatory benefits).
- Dinner: Quinoa stir‑fry with broccoli, kale, and tofu, seasoned with turmeric and ginger.
- Evening beverage: Warm green tea (rich in catechins) with a splash of lemon.
Swap out salmon for sardines or mackerel if you’re on a tighter budget - the omega‑3 punch stays.
Lifestyle Tweaks That Amplify Dietary Gains
Food is only part of the puzzle. Pair your diet with these habits for a smoother skin journey:
- Stay hydrated. Aim for about 2 L of water daily; proper hydration supports the skin barrier.
- Manage stress. Chronic cortisol spikes can mess with immune regulation, worsening psoriasis.
- Prioritize sleep. 7‑9 hours helps skin repair cycles.
- Gentle skin care. Use fragrance‑free moisturizers and avoid harsh scrubs that can strip the protective lipids you’re feeding it.
When to Call a Dermatologist
If you notice any of these red flags, professional help is a smart move:
- Rapid spreading of plaques or sudden pain.
- Bleeding, cracking, or signs of infection.
- Unexplained weight loss or fatigue alongside skin changes - could indicate an underlying autoimmune issue.
Most dermatologists will work with you to combine topical or systemic treatments with a tailored nutrition plan, ensuring you tackle the problem from both inside and out.
Quick Checklist for Skin‑Friendly Eating
- Load up on omega‑3 rich fish or plant sources at least twice a week.
- Include a vitamin‑D source daily (fortified milk, sunlight exposure, or supplement).
- Choose low‑glycemic carbs: quinoa, sweet potatoes, legumes.
- Limit processed meats, sugary drinks, and excessive dairy.
- Track your meals for a few weeks; note any skin changes after specific foods.
Frequently Asked Questions
Can eliminating gluten really improve psoriasis?
For about 10‑15 % of people with psoriasis, gluten sensitivity amplifies inflammation. A short‑term gluten‑free trial (3-4 weeks) can reveal whether plaques soften. If you notice improvement, consider staying gluten‑free long term.
Are supplements necessary if I eat a balanced diet?
Most nutrients can be obtained from foods, but vitamin D and omega‑3 levels often fall short, especially in colder climates like Adelaide. A modest supplement (e.g., 1,000 IU vitamin D and 1 g EPA/DHA) is a safe safety net.
How quickly can I see skin changes after adjusting my diet?
Skin turnover in psoriasis is about 3‑4 days, so some improvement can appear within a week. Full benefits, especially for chronic conditions, usually emerge after 4‑8 weeks of consistent eating.
Is sugar the main villain for all scaly skin conditions?
Sugar fuels inflammation, but its impact varies. It’s a major trigger for psoriasis and seborrheic dermatitis, while keratosis pilaris is less sugar‑sensitive and more linked to dry skin and vitamin A levels.
Should I avoid all dairy if I have eczema?
Not necessarily. Some eczema sufferers react to the whey protein, while others tolerate fermented dairy like kefir. An elimination trial (2 weeks) helps pinpoint your personal trigger.
By paying attention to what lands on your plate, you give your skin the best chance to stay smooth, calm, and free of excess scaling. Ready to try a few swaps today?

Dante Russello
October 23, 2025 AT 15:36First of all, thank you for sharing such a thorough breakdown,; the way you linked omega‑3s, vitamin D, and gut health together is especially helpful; many of us have struggled to connect the dots, and this post makes it crystal clear,; remember to keep a food journal, because tracking triggers can be a game‑changer,; also, don’t forget that hydration plays a surprisingly big role in skin barrier function,; finally, feel free to experiment with different sources of probiotics, such as kefir or fermented veggies, to see what your gut prefers.
sara fanisha
November 1, 2025 AT 20:49Love the practical meal plan-definitely going to try the salmon salad tomorrow!
Jinny Shin
November 11, 2025 AT 03:02One cannot help but marvel at the symphonic interplay between dietary polyphenols and keratinocyte proliferation; the author has orchestrated a culinary concerto that would make even the most discerning epicure swoon; yet, I must caution that the occasional indulgence in nightshades may unleash a tempest of lectin‑induced irritation upon the most fragile epidermis.
deepak tanwar
November 20, 2025 AT 09:16While the optimism is commendable, the assertion that a single salmon salad can drastically alter psoriatic plaques oversimplifies a multifactorial pathology; systemic inflammation, genetic predisposition, and environmental stressors also wield considerable influence, and thus reliance on dietary tweaks alone may foster false hope.
Abhishek Kumar
November 29, 2025 AT 15:29Seems like another diet hype piece.
Heather ehlschide
December 8, 2025 AT 21:42The relationship between nutrition and inflammatory skin disorders has been substantiated by a growing body of clinical research.
The in particular, randomized controlled trials have demonstrated that supplementation with 1–2 g of EPA/DHA per day can reduce PASI scores in moderate psoriasis by up to 20 %.
Moreover, vitamin D status correlates inversely with disease severity, likely due to its role in modulating T‑cell differentiation.
For patients residing at higher latitudes, a daily intake of 1,000–2,000 IU of cholecalciferol is often necessary to achieve serum levels above 30 ng/mL.
Equally important is the impact of the gut microbiome, where dysbiosis has been linked to heightened Th‑17 responses that exacerbate skin inflammation.
Probiotic strains such as Lactobacillus rhamnosus GG and Bifidobacterium longum have shown promise in small pilot studies, reducing erythema and scaling.
When constructing a meal plan, prioritize low‑glycemic carbohydrates; foods like quinoa, lentils, and sweet potatoes avoid the insulin spikes that can amplify inflammatory cytokines.
Saturated fats from processed meats should be limited, as they serve as precursors for arachidonic acid, a substrate for pro‑inflammatory eicosanoids.
On the other hand, monounsaturated fats from olive oil and nuts not only improve lipid profiles but also provide antioxidant polyphenols that protect keratinocytes from oxidative stress.
Green tea catechins, curcumin, and resveratrol are additional phytochemicals with documented anti‑inflammatory mechanisms that can be incorporated through beverages and spices.
It is also wise to assess individual food sensitivities; an elimination diet focusing on gluten, dairy, and nightshades over a three‑week period can reveal hidden triggers in up to 15 % of patients.
Patients should document daily intake alongside flare severity using a simple visual analogue scale to identify patterns over time.
Consistency is key-most clinicians observe measurable improvement after four to eight weeks of sustained dietary adherence.
Nonetheless, diet should complement, not replace, evidence‑based pharmacotherapy, as systemic agents remain the cornerstone for severe disease.
Collaboration between dermatologists, dietitians, and primary care providers ensures that nutritional interventions are safe, especially when patients are on immunosuppressive medications.
In summary, a balanced approach that includes omega‑3 fatty acids, adequate vitamin D, a diverse array of antioxidants, and personalized elimination testing can markedly enhance skin outcomes when paired with conventional treatment.
Dan Danuts
December 18, 2025 AT 03:56Great points! I’ve been swapping out my usual cheese for kefir lately, and the itchiness has noticeably mellowed-high‑five to anyone else giving gut‑friendly foods a shot!
Scott Ring
December 27, 2025 AT 10:09Coming from the Midwest, I never realized my love for fried chicken could be messing with my scalp; swapping the batter for a herb‑spiced baked version cut down the flakes on my shoulders without sacrificing flavor.
Shubhi Sahni
January 5, 2026 AT 16:22That’s a fantastic example,; you’ve illustrated how a simple cooking technique alteration can yield impressive dermatological benefits,; many readers will appreciate the concrete swap,; keep experimenting, and share your results!
Danielle St. Marie
January 14, 2026 AT 22:36Honestly, if you’re still munching on processed snacks while preaching skin health, you’re missing the point 😒. True transformation requires disciplined eating, not half‑hearted attempts.
keerthi yeligay
January 24, 2026 AT 04:49i get u but maybe start small r not all at once
Peter Richmond
February 2, 2026 AT 11:02The interplay between micronutrients and epidermal turnover underscores the necessity of evidence‑based dietary recommendations in dermatological practice.
Bonnie Lin
February 11, 2026 AT 14:36Thanks for the clear guide.