When you pick up a prescription, you might not think about how much it costs the system-until you see the price tag. But here’s the truth: generic drugs are one of the biggest reasons prescription drug spending hasn’t exploded even as more people need medication. The real question isn’t whether generics work-it’s whether we’re picking the right ones, at the right price. Cost-effectiveness analysis (CEA) is how experts figure that out.
What Cost-Effectiveness Analysis Actually Measures
Cost-effectiveness analysis doesn’t just look at the sticker price of a pill. It asks: How much health do we get for every dollar spent? The standard unit is the quality-adjusted life year, or QALY. One QALY means one year of perfect health. If a drug helps someone live an extra year with chronic pain, it might count as 0.7 QALYs. If it restores full health, it’s 1.0. For generics, CEA compares two things: the cost of a drug and the health outcome it delivers. A generic version of a blood pressure pill might cost $5 a month. The brand-name version? $120. Both work the same. The CEA shows the generic delivers the same QALYs for 96% less money. That’s not just savings-it’s a win for patients, insurers, and public health systems.How Generic Prices Crash After Patent Expiry
The moment a brand-name drug loses patent protection, prices don’t just drop-they collapse. According to the FDA, the first generic competitor cuts the price by about 39%. When six or more generics hit the market, prices fall more than 95% below the original brand price. Here’s what that looks like in practice:- One generic competitor: 54% cheaper than the brand
- Two generics: 67% cheaper
- Four generics: 79% cheaper
- Six or more: over 95% cheaper
The Hidden Problem: High-Cost Generics
Here’s the twist: not all generics are cheap. A 2022 study in JAMA Network Open looked at the top 1,000 generic drugs and found 45 that were wildly overpriced-15.6 times more expensive than other drugs in the same therapeutic class. One example: a generic version of a common cholesterol drug was priced at $2,400 per year. But another generic in the same class, with the same active ingredient and same effectiveness, cost just $150. That’s a 94% difference. Why does this happen? The answer isn’t science. It’s market structure. Pharmacy Benefit Managers (PBMs) often profit from “spread pricing”-they negotiate a high price with pharmacies, pay insurers less, and pocket the difference. So even when a cheaper generic exists, the system keeps paying more because someone’s making money off the gap.
Therapeutic Substitution: The Secret Savings Tool
Sometimes, the best way to save isn’t to pick a cheaper version of the same drug. It’s to pick a different drug entirely that works just as well. The same JAMA study found that switching from a high-cost generic to a lower-cost drug in the same therapeutic class could cut spending by nearly 90%. For example:- Switching from a $2,400 generic statin to a $150 alternative saved $2,250 per patient per year.
- Across the 45 high-cost generics studied, total spending dropped from $7.5 million to just $873,711 when swapped out.
Why Most Cost-Effectiveness Studies Get It Wrong
Here’s the shocking part: 94% of published cost-effectiveness analyses don’t account for what happens after a drug goes generic. They assume prices stay high forever. That’s like predicting a car’s fuel efficiency based on its sticker price-ignoring the fact that it’ll be on sale for half off next year. When analysts ignore patent cliffs, they make new drugs look more cost-effective than they really are. That pushes decision-makers toward expensive brands, even when generics are coming. The National Institutes of Health (NIH) warned in 2023 that this creates a dangerous bias. If you don’t model the drop in price after generic entry, you’ll reject drugs that are actually the best long-term value. That’s not just a mistake-it’s a financial trap.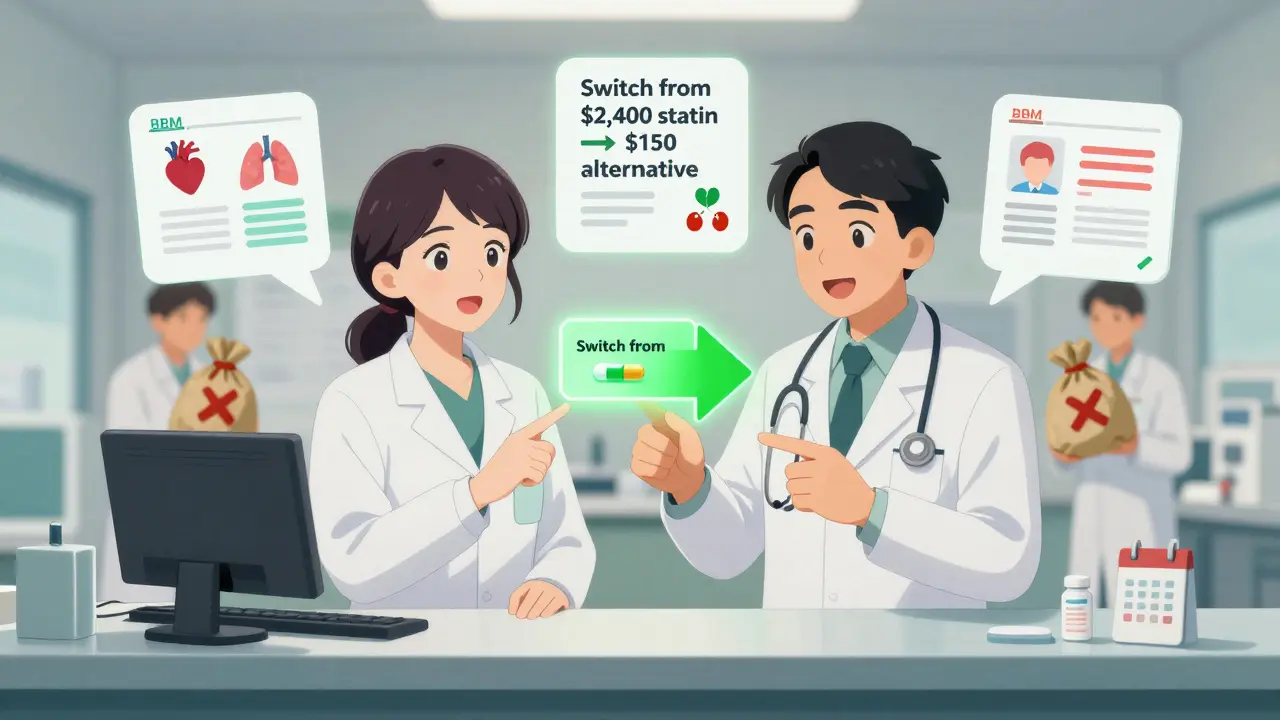
How Different Countries Handle It
In Europe, over 90% of health technology assessment agencies use formal cost-effectiveness analysis to decide which drugs get covered. They update their models regularly as generics enter the market. In the U.S., only 35% of commercial insurers do the same. Medicare Part D, which covers 40 million seniors, still relies heavily on formularies shaped by PBM deals-not health economics. The difference shows up in outcomes. Countries that use CEA to guide generic substitution spend less per capita on drugs and get better population health. The U.S. spends more than any other country on prescription drugs-and still has worse outcomes on many chronic conditions.What Needs to Change
There are three clear steps to fix this:- Update CEA models to include future generic pricing. Analysts need to forecast when patents expire and how many generics will enter. Tools exist. They just aren’t being used.
- Remove spread pricing incentives. PBMs should be paid a flat fee, not a percentage of the drug price. That removes the motive to keep expensive generics on formularies.
- Require therapeutic substitution alerts. Pharmacy systems should flag when a cheaper alternative exists-even if it’s a different drug. Pharmacists need real-time data to make the right call at the counter.
What Patients Can Do
You don’t need to be an economist to save money. Here’s what works:- Ask your pharmacist: “Is there a cheaper version of this drug in the same class?”
- Check GoodRx or SingleCare before filling a prescription. Prices vary wildly between pharmacies.
- Don’t assume “generic” means cheap. Compare the price of your generic to others for the same condition.
- If your drug costs more than $200 a month and you’re on a fixed income, ask about patient assistance programs. Many manufacturers offer them-even for generics.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and performance. Bioequivalence studies prove they work the same way in the body. The only differences are in inactive ingredients-like fillers or dyes-which don’t affect how the drug works.
Why are some generic drugs so expensive?
Some generics are expensive because of market distortions, not cost. Pharmacy Benefit Managers (PBMs) sometimes profit from the difference between what they charge insurers and what they pay pharmacies-a practice called spread pricing. This creates an incentive to keep higher-priced generics on formularies, even when cheaper alternatives exist. Also, if only one or two companies make a generic, competition is low and prices stay high.
What is therapeutic substitution?
Therapeutic substitution means switching from one drug to another in the same class that works just as well but costs less. For example, swapping a high-cost generic statin for a lower-cost one. It’s not about lowering quality-it’s about matching value. Studies show this can cut drug costs by up to 90% without affecting patient outcomes.
Does cost-effectiveness analysis favor big pharmaceutical companies?
Not if done right. But many studies are funded by drugmakers and use outdated pricing assumptions-like ignoring future generic competition. This makes new branded drugs look more cost-effective than they are. Independent analyses, like those from ICER or government agencies, are more reliable because they include realistic price projections and compare all available options, including generics.
How can I find out if my generic drug has a cheaper alternative?
Use tools like GoodRx, SingleCare, or the VA’s National Formulary. These show price comparisons across pharmacies and sometimes list therapeutic alternatives. You can also ask your pharmacist directly: “Is there a lower-cost drug in the same class that works just as well?” Pharmacists often know more than doctors about pricing options.

Dusty Weeks
January 1, 2026 AT 14:51Layla Anna
January 2, 2026 AT 16:48LIZETH DE PACHECO
January 4, 2026 AT 13:23Olukayode Oguntulu
January 5, 2026 AT 17:27jaspreet sandhu
January 6, 2026 AT 18:51Heather Josey
January 7, 2026 AT 20:47sharad vyas
January 9, 2026 AT 07:35Bill Medley
January 9, 2026 AT 08:43Stephen Gikuma
January 9, 2026 AT 11:34Alex Warden
January 11, 2026 AT 00:58Lee M
January 12, 2026 AT 14:53Bobby Collins
January 13, 2026 AT 13:03