When you're diagnosed with celiac disease, the focus is usually on gut symptoms-bloating, diarrhea, fatigue. But what if your liver enzymes are high, and your doctor says there's no alcohol use, no hepatitis, no obesity? That’s not uncommon. In fact, up to 40% of people with untreated celiac disease show abnormal liver tests. And here’s the twist: those numbers often go back to normal-not with pills or injections-but just by cutting out gluten.
Why Does Celiac Disease Affect the Liver?
Celiac disease isn’t just a digestive issue. It’s an autoimmune condition where the body attacks its own small intestine after eating gluten. But that immune response doesn’t stop at the gut. It can spill over, triggering inflammation elsewhere-including the liver. Studies show that about 36.7% of celiac patients have elevated liver enzymes (ALT and AST), compared to just 19.3% in people without celiac. That’s nearly double. The most common pattern? Both ALT and AST rise together, which points to liver cell damage rather than bile duct problems. The connection isn’t random. Three main mechanisms are at play:- Leaky gut: Damaged intestinal lining lets toxins and undigested food particles slip into the bloodstream and reach the liver. The liver, trying to filter them out, gets inflamed.
- Autoimmune cross-reaction: The immune system, already on high alert for gluten, sometimes mistakes liver proteins for gluten fragments. This can lead to autoimmune hepatitis, which occurs in 4-6.4% of celiac patients.
- Nutrient malabsorption: Without healthy villi, fat-soluble vitamins like A, D, E, and K aren’t absorbed. Vitamin E, for example, is a powerful antioxidant that protects liver cells. Low levels mean less protection.
What Liver Conditions Are Linked to Celiac Disease?
Celiac disease doesn’t just cause vague enzyme spikes. It’s tied to specific liver conditions:- Autoimmune hepatitis: The liver attacks itself. About 1 in 20 people with autoimmune hepatitis also have celiac disease.
- Primary biliary cholangitis and primary sclerosing cholangitis: These are rarer but well-documented. Both involve bile duct damage, and celiac patients are at higher risk.
- MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease): Formerly called NAFLD, this is fatty liver not caused by alcohol. It’s surprisingly common in celiac patients-up to 50% show signs of fat buildup in liver tissue on biopsies.
How Common Is This, Really?
A 2025 meta-analysis compared siblings-one with celiac disease, one without. The results were stark: celiac patients had double the risk of chronic liver disease. Even more telling: 4.7% of people with unexplained cirrhosis (called cryptogenic cirrhosis) turned out to have undiagnosed celiac disease. That’s why guidelines now recommend screening for celiac disease in anyone with unexplained liver enzyme elevations-even if they feel fine. Many patients don’t have digestive symptoms at all. Fatigue, joint pain, or just a weird blood test might be the only clues.
Can It Be Reversed?
Yes. And that’s the most hopeful part. Research from Beth Israel Deaconess Medical Center shows that 79% of celiac patients with abnormal liver enzymes see them return to normal within 12 to 18 months of a strict gluten-free diet. Some see improvement in as little as 3 months. One patient on Reddit shared: “My ALT was 142 when I got diagnosed. Doctors thought it was fatty liver. Then they found my tTG antibodies. After 6 months gluten-free? Down to 38.” But here’s the catch: not everyone improves. If liver enzymes stay high after a year of no gluten, doctors need to look for something else-like autoimmune hepatitis or primary biliary cholangitis. That’s why follow-up blood tests every 3-6 months are critical.What Should You Do If You Have Celiac Disease and High Liver Enzymes?
Step 1: Get tested. If you’ve just been diagnosed with celiac disease, ask for a full liver panel: ALT, AST, ALP, bilirubin, and GGT. Don’t assume it’s nothing. Step 2: Go gluten-free-really gluten-free. Even small amounts of cross-contamination can keep the immune system active and the liver inflamed. Read labels. Use separate toasters. Avoid shared fryers. Step 3: Eat real food. Skip the gluten-free cookies, pasta, and snacks. Focus on vegetables, fruits, lean meats, eggs, legumes, nuts, seeds, and whole gluten-free grains like quinoa, buckwheat, and brown rice. These support liver repair, not fat buildup. Step 4: Work with a dietitian who knows celiac disease. A 2023 study found patients who got specialized nutrition counseling normalized their liver enzymes 30% faster than those who didn’t. Step 5: Monitor. Repeat liver tests every 3-6 months until levels stabilize. Then once a year after that.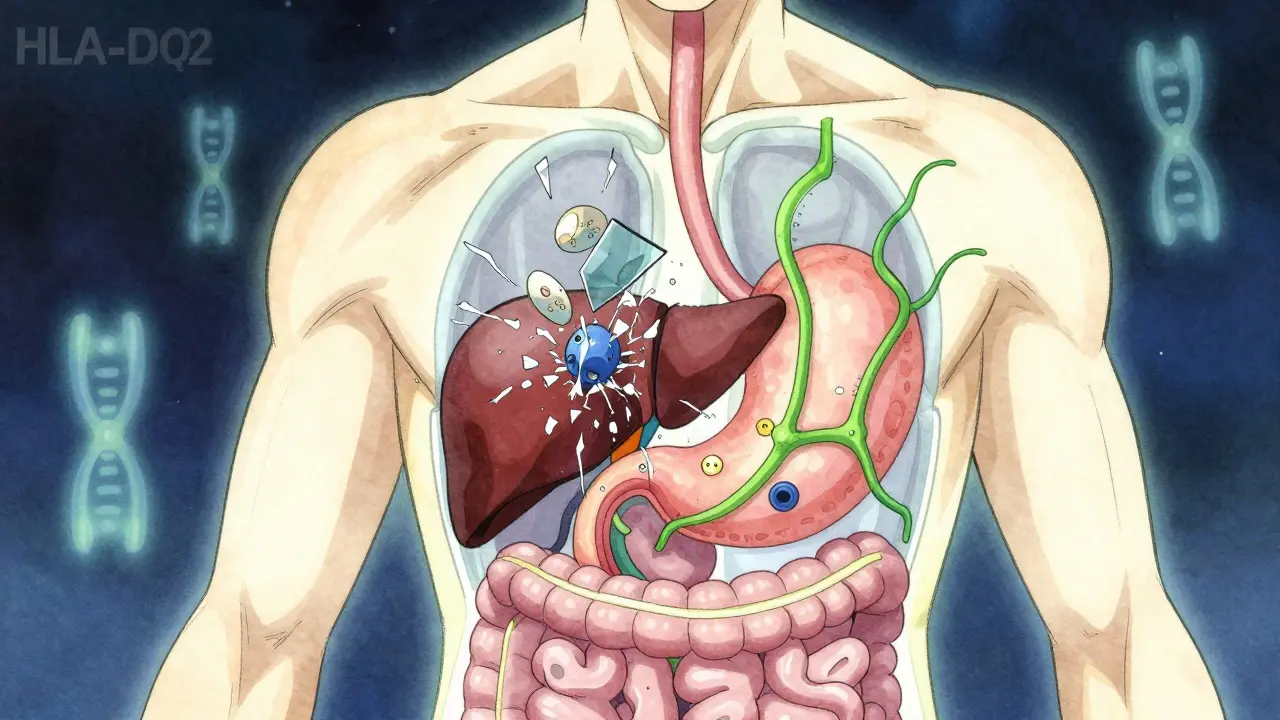
What’s Changing in Medical Practice?
Five years ago, only 65% of doctors ordered liver tests when diagnosing celiac disease. Today, that number is 92%. Why? Because the evidence became impossible to ignore. In June 2024, the European Association for the Study of the Liver updated its guidelines to say: Screen all patients with cryptogenic cirrhosis for celiac disease. That’s a big deal. It means doctors now treat abnormal liver tests as a possible red flag for celiac-not just a side note. Researchers are also exploring genetic markers. Early data from Mayo Clinic suggests people with two copies of the HLA-DQ2 gene (homozygous) are 2.3 times more likely to develop liver problems than those with just one copy. And there’s new hope on the horizon. Takeda Pharmaceutical’s Phase II trial, completed in late 2023, tested an enzyme therapy designed to break down gluten in the stomach before it reaches the intestine. If it works, it could reduce liver inflammation in celiac patients-even if they accidentally eat gluten.What’s the Bottom Line?
Celiac disease and liver abnormalities are deeply connected-not just by coincidence, but by biology. The liver doesn’t just sit there quietly. It reacts to what’s happening in the gut. And when gluten is the trigger, the damage is often reversible. You don’t need a liver specialist to fix this. You need a gluten-free diet, real food, and consistency. Most people see their liver heal without medication. But you have to be strict. You have to be patient. And you have to get tested if something feels off. This isn’t just about your gut anymore. It’s about your whole body. And your liver? It’s watching. Waiting. Ready to heal-if you give it the chance.Can celiac disease cause elevated liver enzymes even if I have no digestive symptoms?
Yes. Many people with celiac disease have no classic gut symptoms like diarrhea or bloating. Instead, they might only notice fatigue, joint pain, or abnormal liver tests. In fact, up to 40% of untreated celiac patients show elevated liver enzymes without any gastrointestinal complaints. This is why doctors now screen for celiac disease in people with unexplained liver enzyme elevations-even if they feel fine.
Will my liver enzymes go back to normal on a gluten-free diet?
For most people, yes. Studies show that about 79% of celiac patients with abnormal liver enzymes see them return to normal within 12 to 18 months of strictly avoiding gluten. Some see improvements in as little as 3 months. The liver has a strong ability to repair itself when the trigger-gluten-is removed. However, if enzymes remain high after a year, further testing for other liver conditions like autoimmune hepatitis is needed.
Can going gluten-free actually cause fatty liver?
Yes, paradoxically. Many processed gluten-free products are high in sugar, refined starches, and unhealthy fats to mimic the texture of bread and pasta. Eating too much of these can lead to weight gain and fat buildup in the liver-known as MASLD. This is why experts recommend focusing on whole, unprocessed foods like vegetables, fruits, lean proteins, and whole gluten-free grains instead of packaged gluten-free snacks.
Should I get tested for celiac disease if I have fatty liver and no other symptoms?
If your fatty liver is unexplained (not linked to obesity, alcohol, or diabetes), yes. Research shows that 4.7% of people with cryptogenic cirrhosis-liver scarring with no clear cause-have undiagnosed celiac disease. Even mild, persistent liver enzyme elevations warrant testing, especially if you have a family history of autoimmune conditions. A simple blood test for tTG-IgA antibodies can rule it in or out.
What’s the difference between celiac-related liver damage and alcoholic liver disease?
The biggest difference is reversibility. Celiac-related liver damage often improves completely with a gluten-free diet alone, without the need for medications or lifestyle changes beyond food. Alcoholic liver disease requires stopping alcohol, and damage may be permanent if advanced. Also, celiac-related liver issues usually involve mild to moderate enzyme elevations (2-5 times normal), while alcoholic disease often causes much higher spikes. Blood tests can also check for celiac antibodies, which won’t be present in alcohol-related cases.
How often should liver enzymes be checked after a celiac diagnosis?
At diagnosis, get a full liver panel. Then repeat every 3-6 months until enzymes normalize, which usually happens within 12 months for 85% of patients. Once normal, annual checks are sufficient unless symptoms return or new issues arise. If enzymes don’t improve after a year on a strict gluten-free diet, your doctor should investigate for coexisting autoimmune liver diseases like autoimmune hepatitis or primary biliary cholangitis.
Kelly Mulder
December 19, 2025 AT 09:42The notion that gluten-free processed foods are worse for the liver than their gluten-containing counterparts is not merely a dietary observation-it’s a systemic indictment of the industrial food complex. We’ve replaced one toxin with another, disguised as ‘health.’ The industry profits from fear, not healing. And yet, we’re told to ‘just eat clean’ as if the burden of corporate malfeasance lies with the consumer. The liver doesn’t care about your intentions-it only responds to molecular structure. And refined tapioca starch? It’s just sucrose in a trench coat.
Dominic Suyo
December 20, 2025 AT 21:15So let me get this straight-we’re supposed to believe that a diet that’s basically just carbs with a different name is somehow magically healing? The liver doesn’t give a damn if it’s gluten or gluten-free corn syrup. This whole narrative is a placebo wrapped in a lab coat. 79% improvement? That’s probably just regression to the mean and people finally stopping their 12-packs-a-week soda habit under the guise of ‘gluten-free wellness.’
Janelle Moore
December 21, 2025 AT 20:52Did you know the government is secretly adding glyphosate to gluten-free products to make people sick so they buy more meds? My cousin’s neighbor’s dog got liver cancer after eating gluten-free kibble. It’s all connected. They don’t want you to heal. They want you dependent. Check the labels-look for ‘natural flavors’-that’s code for poison.
Henry Marcus
December 23, 2025 AT 11:42Wait-so if you’re homozygous for HLA-DQ2, and you eat a gluten-free muffin from a shared toaster, and your ALT spikes again… is that a biological signal… or is it a cosmic reminder that you’re still not pure enough? I’ve been gluten-free for 11 years. My liver’s fine. But my soul? It’s still haunted by the ghost of wheat.
Carolyn Benson
December 23, 2025 AT 16:15There’s a deeper metaphysical truth here: the liver is the organ of judgment. When it reacts to gluten, it’s not just processing toxins-it’s processing guilt. The modern world is a lie. We eat to numb. We avoid gluten not to heal, but to perform wellness. The real disease isn’t celiac-it’s the belief that we can outsource healing to a diet. The liver knows. It remembers. And it will not be fooled by quinoa.
Chris porto
December 25, 2025 AT 07:18I’ve seen this in my clinic. People come in with crazy high ALT, no symptoms, no alcohol, no obesity. We test for celiac-positive. Go gluten-free. Six months later, enzymes normal. No meds. Just food. It’s not magic. It’s biology. And yeah, processed gluten-free stuff is trash. But real food? That’s the cure. Simple. No conspiracy. Just science. And patience.
holly Sinclair
December 27, 2025 AT 04:51It’s fascinating how the body doesn’t compartmentalize. The gut isn’t a separate room-it’s the front door to the entire system. When the intestinal barrier breaks down, it’s not just food particles leaking-it’s identity, trauma, immune memory, all of it spilling into circulation. The liver doesn’t see ‘gluten’-it sees ‘invasion.’ And it responds not as a filter, but as a sentinel. That’s why recovery isn’t just about removing gluten-it’s about restoring the integrity of the entire terrain. We treat organs like machines, but they’re ecosystems. And ecosystems heal when the conditions are right-not when you slap on a label that says ‘gluten-free.’
Monte Pareek
December 27, 2025 AT 05:35Listen. If you’ve got celiac and high liver enzymes, you’ve got a roadmap. Step one: stop eating crap labeled gluten-free. Step two: eat real food. Step three: get a dietitian who doesn’t sell you bars. Step four: test every 3 months. Step five: breathe. You don’t need a miracle. You need consistency. I’ve had patients go from ALT 200 to 40 in 4 months. No drugs. Just food. And yes, it’s hard. But your liver? It’s been waiting for you to show up. It’s not broken. It’s just been starved of peace.
Tim Goodfellow
December 27, 2025 AT 17:54Bro. My buddy had cryptogenic cirrhosis. No alcohol. No fat. No diabetes. Then they found celiac. Went gluten-free. Two years later, his biopsy showed NO fibrosis. Zero. Just… gone. Like it never happened. That’s not a fluke. That’s a revolution in a grocery aisle. Stop overthinking. Just eat the damn vegetables.
Takeysha Turnquest
December 28, 2025 AT 21:56The liver is the silent witness. It doesn’t scream. It doesn’t beg. It just… holds the truth. And when you finally stop poisoning it with lies disguised as food-it doesn’t thank you. It just… heals. Quietly. Efficiently. Like it always knew how. You didn’t cure it. You just stopped hurting it.
Lynsey Tyson
December 30, 2025 AT 21:01Just wanted to say thank you for this. I was diagnosed last year with celiac and my ALT was 145. I thought I was doomed. Started eating real food-no gluten-free bread, just eggs, spinach, chicken, sweet potatoes. Six months later, normal. I didn’t know it could be this simple. You’re right-it’s not about the diet. It’s about the truth.