When you have bronchiectasis, your lungs don’t clear mucus the way they should. The airways become widened, flabby, and scarred - not from one bad infection, but from years of repeated cycles: mucus builds up, bacteria grow, your body fights back, and the damage gets worse. It’s not just a cough. It’s a daily battle - with thick, foul-smelling sputum, constant fatigue, and the fear of the next flare-up. But here’s the truth: bronchiectasis isn’t a death sentence. It’s a condition you can manage - if you know how to break the cycle.
What Bronchiectasis Really Means
Bronchiectasis isn’t a single disease. It’s the result of long-term damage to the bronchial tubes - the airways that carry air in and out of your lungs. Think of them like garden hoses. If they’re constantly clogged, swollen, or infected, they stretch out and lose their shape. Once they’re stretched, they can’t snap back. That’s when mucus starts pooling. And pooled mucus? It’s a breeding ground for bacteria.
Most people don’t realize they have it until they’ve had a chronic cough for months or years. You might brush it off as a smoker’s cough, a lingering cold, or just getting older. But if you’re coughing up 30 milliliters or more of yellow or green sputum every day - especially if it smells bad - that’s a red flag. Chest CT scans are the gold standard for diagnosis. Doctors look for one clear sign: the bronchial artery is at least 1.5 times wider than the pulmonary artery next to it. That’s not normal. That’s damage.
In the U.S., about 350,000 people have been diagnosed. But experts believe many more are undiagnosed. It’s especially common in people over 75, and it affects roughly 1 in 1,000 adults overall. It’s not just about age, though. It can follow pneumonia, tuberculosis, immune disorders, or even untreated asthma. And while cystic fibrosis can cause it, most cases - over 80% - are not linked to CF.
The Daily Battle: Chronic Cough and Sputum
Let’s talk about the cough. It’s not the kind that goes away after a week. This is a deep, rattling cough that wakes you up at night, makes your ribs ache, and leaves you exhausted. The sputum? It’s not clear. It’s thick. It’s often green or yellow because of all the white blood cells fighting infection. Some people produce a cupful a day. Others, more.
And here’s the cruel twist: the more you cough, the more your airways get irritated. The more irritated they are, the more mucus they make. That’s the cycle. It doesn’t stop unless you break it.
Studies show that without treatment, your lung function - measured by FEV1 (how much air you can blow out in one second) - drops by 30 to 50 mL every year. That’s twice as fast as normal aging. If you do nothing, you’re on track for more hospital visits, more antibiotics, and eventually, oxygen therapy. About 15 to 20% of patients end up needing oxygen. Five percent will need surgery.
Why Antibiotics Alone Don’t Work
It’s tempting to think antibiotics are the answer. You cough, you feel sick, you take a course. But here’s what most people don’t know: using antibiotics only during flare-ups makes things worse.
A 2021 European Respiratory Society report found that patients who only took antibiotics during infections had 2.3 times higher risk of permanent lung damage than those on consistent, full-management plans. Why? Because you’re not removing the mucus. You’re just killing some bacteria - and leaving the rest behind. The survivors? They get stronger. They become resistant.
Research from MedlinePlus shows that 38% of bronchiectasis patients develop antibiotic-resistant bacteria within five years of chronic antibiotic use. That’s not rare. That’s predictable. And once you have resistant strains like Pseudomonas aeruginosa, your treatment options shrink fast.
Long-term, low-dose antibiotics can help - but only if paired with airway clearance. Azithromycin, taken 3 times a week at 250-500 mg, reduces flare-ups by 32% compared to placebo. But that’s not because it’s a magic bullet. It’s because it has anti-inflammatory effects and helps control bacteria. Still, it’s not a standalone fix.

The Real Game-Changer: Sputum Clearance
If you remember one thing from this article, remember this: airway clearance is not optional. It’s as essential as taking antibiotics. That’s not a slogan. That’s what Dr. Shivani Gupta at Penn Medicine says - and she’s one of the top experts in the field.
Patients who do daily airway clearance have 47% fewer hospitalizations each year. That’s not a guess. That’s from a 2023 study at UT Southwestern. And here’s the kicker: those who skip it lose lung function 45 mL per year - nearly double the rate of those who stick to their routine.
There are several proven techniques:
- Active Cycle of Breathing Techniques (ACBT): A sequence of breathing control, thoracic expansion, and huff coughing. It’s taught by respiratory therapists and works for most people.
- Huff Coughing: Not a regular cough. It’s a forced exhalation from the chest, like you’re trying to fog up a mirror. You do it at different lung volumes - high, medium, low. Done right, it moves mucus without triggering a violent cough. 78% of patients on the American Lung Association forum say this gives them immediate relief.
- Positive Expiratory Pressure (PEP) Devices: Tools like the Aerobika® or Flutter valve. You breathe out through a resistance, which creates pressure that keeps airways open and pushes mucus up. Studies show they’re just as effective as expensive oscillating vests - but cost $150 instead of $7,000.
- High-Frequency Chest Wall Oscillation (HFCWO): The vest. It vibrates your chest 20-25 times per second. It’s effective - 35% more sputum cleared than traditional methods - but it’s expensive and not always covered by insurance.
Most people need 15 to 20 minutes, once or twice a day. Some need longer. The key isn’t perfection. It’s consistency. Patients who stick with it for 6-8 weeks report major improvements. The first few weeks? Frustrating. You’ll feel like you’re not getting anywhere. But after that, you’ll notice less coughing, less shortness of breath, fewer sick days.
What Else Helps: Nebulizers, Hydration, and More
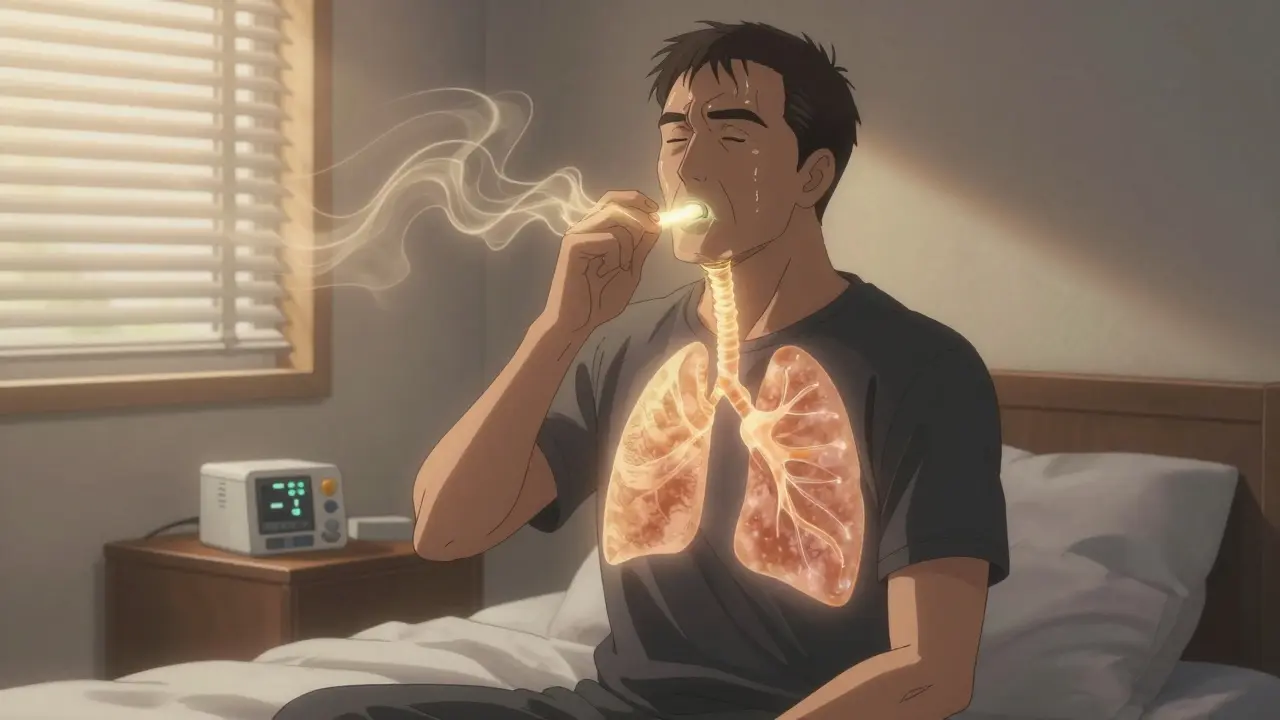
Clearing mucus is easier when it’s thinner. That’s where nebulizers come in.
- Hypertonic saline (7%): A saltwater mist that draws water into the airways, thinning mucus. 3 mL daily is standard. Many patients report it’s the single most helpful tool in their routine.
- Dornase alfa (Pulmozyme): Originally for cystic fibrosis, it breaks down DNA from dead white blood cells in mucus. It’s used off-label for bronchiectasis and can help if your sputum is thick and stringy.
- Inhaled antibiotics: Tobramycin (300 mg twice daily) cuts Pseudomonas colonization by 56%. It’s not for everyone, but if you have chronic Pseudomonas, it’s a game-changer.
Hydration matters more than you think. Drink at least 2 liters of water a day. It sounds simple, but dehydration makes mucus stickier. Alcohol and caffeine? They dry you out. Limit them.
Bronchodilators? They don’t fix bronchiectasis. But if you also have wheezing or tightness, using an inhaler like albuterol before your airway clearance can help open your airways - and make your techniques 28% more effective.
Real-Life Challenges: Adherence, Cost, and Support
Here’s the ugly truth: most people don’t stick with it.
42% of NHS users say they struggle to fit 20-minute daily routines into work, childcare, or caregiving. 55% need retraining within six months because they forget how to huff properly. Insurance doesn’t always cover devices. The Aerobika® costs $150-$200. The vest? $5,000-$7,000. Medicare requires you to have more than 3 flare-ups a year to cover long-term antibiotics. Medicaid patients have 3.2 times more hospitalizations - not because they’re less sick, but because they can’t access therapy.
But there’s hope. The American Thoracic Society’s “Clearing the Air” app helps track daily routines. The Bronchiectasis and NTM Initiative runs free monthly virtual support groups. Reddit’s r/Bronchiectasis community has over 1,800 members sharing tips. One patient went from 9 hospital stays a year to 1 after starting daily hypertonic saline and ACBT. That’s not luck. That’s discipline.
The Future: What’s Next
Science is moving fast. In 2023, the FDA approved gallium maltolate - an inhaled treatment for stubborn Pseudomonas infections. It cut flare-ups by 42% in trials. Researchers are now testing bacteriophages (viruses that kill bacteria) for antibiotic-resistant strains. Early results show 68% eradication rates. Genetic markers are being identified to predict who’ll progress faster - so treatment can be personalized by 2025.
But no new drug will fix what you don’t clear. No pill will replace the huff cough. The best treatment today is still the same: daily airway clearance, smart antibiotic use, and staying hydrated. It’s not glamorous. But it works.
Can bronchiectasis be cured?
No, bronchiectasis cannot be cured. The structural damage to the airways is permanent. But with consistent management - especially daily airway clearance and appropriate antibiotics - you can stop the cycle of infection and inflammation. Many people live full, active lives with minimal symptoms.
How do I know if I’m doing airway clearance right?
You should feel mucus moving up and be able to cough it out without wheezing or extreme fatigue. If you’re not producing sputum after 15 minutes, you might not be doing it correctly. A respiratory therapist can watch you for 3-4 sessions and correct your technique. Look for signs like less coughing later in the day, less green sputum, and fewer flare-ups.
Is it safe to take antibiotics long-term?
Yes - but only under medical supervision. Long-term, low-dose azithromycin (three times a week) is proven to reduce flare-ups and inflammation. But it’s not a substitute for airway clearance. Combining it with daily clearance reduces the risk of resistance. Your doctor will monitor for side effects like hearing loss or liver issues.
What’s the best device for airway clearance?
There’s no single “best” device. For most people, a handheld PEP device like Aerobika® or Flutter valve works as well as expensive vests - and costs a fraction. If you have trouble using your hands, a vest might be better. If cost or insurance is an issue, PEP devices are the most practical choice. Talk to your respiratory therapist about options.
Can I stop treatment if I feel better?
No. Feeling better doesn’t mean the mucus is gone or the bacteria are gone. Stopping clearance or antibiotics increases your risk of a major flare-up - and permanent lung damage. Bronchiectasis management is lifelong. Think of it like managing high blood pressure: you feel fine, but you still take the pill.
Daniel Dover
February 14, 2026 AT 13:50Consistency is everything. I’ve been doing PEP for 18 months. No more hospital trips. Simple as that.
Virginia Kimball
February 14, 2026 AT 23:59Y’all need to hear this: airway clearance isn’t a chore - it’s your superpower. I used to hate it. Now I treat it like my morning coffee. 15 minutes, twice a day, and suddenly I can breathe through a whole movie without wheezing. No magic pills. Just muscle memory and grit. You got this.
Mike Hammer
February 16, 2026 AT 00:30Been living with this since 2019. The vest was a nightmare to get covered. Ended up buying a Flutter valve on Amazon for $80. Changed everything. Also, hydration. Drink water like it’s your job. I used to chug soda. Now? Herbal tea, lemon water, the whole vibe. My sputum went from thick tar to something you can actually expect to cough up without a war cry.
Sarah Barrett
February 16, 2026 AT 12:40Interesting how the data aligns with clinical practice. The 47% reduction in hospitalizations isn’t anecdotal - it’s replicated across multiple centers. What’s underreported is the psychological burden of daily routines. Many patients abandon therapy not because they’re lazy, but because they’re exhausted - emotionally and physically. We need better support systems, not just better devices.
Chiruvella Pardha Krishna
February 18, 2026 AT 06:57The cycle of mucus, infection, inflammation - it mirrors the metaphysical struggle of existence itself. We are all bronchiectatic in some way. The body, like the soul, becomes scarred by repetition. To clear the airway is not merely medical - it is an act of existential defiance. The antibiotics? A temporary ceasefire. The huff? The scream into the void that somehow, miraculously, works.
Joe Grushkin
February 19, 2026 AT 23:35Y’all are treating this like a wellness trend. Azithromycin? PEP devices? Please. The real solution is avoiding the whole damn system. Stop going to doctors. Stop buying gadgets. Your body knows how to heal. Let it. Modern medicine invented this disease to sell vests. I haven’t done a single clearance in three years. Still breathing. Coincidence? I think not.
Mandeep Singh
February 20, 2026 AT 13:30Let me tell you something about American healthcare. You have 350,000 diagnosed cases? That’s a drop in the bucket. In India, we don’t even have CT scans in half the villages. People die with chronic coughs because they can’t afford a $150 device. You think your insurance issues are bad? Try explaining to a village doctor that you need a ‘high-frequency chest wall oscillation’ when he’s never heard of bronchiectasis. This isn’t a medical issue - it’s a global injustice wrapped in a pulmonary disguise.
Erica Banatao Darilag
February 20, 2026 AT 20:02I’ve been following this for years. I was diagnosed in 2021. At first, I thought I could skip days. I did. I paid for it. Three ER visits in six months. Then I started ACBT with my therapist. It felt ridiculous at first - breathing like a yoga instructor while coughing into a tissue. But after six weeks? I stopped waking up at 3 a.m. with a lung full of sludge. I’m not cured. But I’m not dying either. And that’s enough.
Betty Kirby
February 22, 2026 AT 15:42Anyone else notice how people treat this like it’s optional? It’s not. It’s not a hobby. It’s not a lifestyle tweak. It’s your lungs we’re talking about. If you stop, you’re not ‘taking a break’ - you’re handing your future to bacteria. And don’t even get me started on people who say ‘I feel fine so I’ll skip.’ You don’t feel fine. You’ve just gotten used to being miserable.
Kapil Verma
February 24, 2026 AT 11:15Western medicine is a scam. In my village, we use turmeric, neem, and steam from boiled eucalyptus. No machines. No pills. Just ancestral wisdom. You think a $7,000 vest beats 5000 years of Ayurveda? You’re delusional. This is why your people are sick - you trust machines over nature. I’ve helped 17 patients in my community. Zero hospitalizations. No antibiotics. Just truth.
Michael Page
February 26, 2026 AT 01:46Reading this made me realize something. We’re all just trying to survive a body that refuses to cooperate. I used to think bronchiectasis was my fault - like I failed at being healthy. But it’s not. It’s biology. It’s damage. It’s a system that broke and won’t fix itself. The only thing we control is showing up. Every day. Even when it sucks. Even when you’re tired. Even when you don’t believe it’s working. You show up. And that’s how you win.