Medication Vision Risk Checker
Medication Vision Risk Checker
Enter your medications to see if they may cause blurred vision or eye damage. This tool helps you understand your risk factors.
Your Risk Assessment
Blurred vision isn't always just tired eyes or needing new glasses. For millions of people taking common medications, it’s a warning sign - one that can sneak up quietly and lead to permanent damage if ignored. You might not connect your blurry vision to the pill you take every morning, but dozens of widely prescribed drugs can directly affect your eyes. The good news? Most of these side effects are preventable if you know what to watch for and when to act.
Why Your Medication Might Be Blurring Your Vision
Your eyes are delicate organs, and many medications don’t just target the problem area - they affect everything they touch. Blurred vision from drugs happens through several different mechanisms, each tied to specific medications and risk levels.
Some drugs dry out your eyes. Isotretinoin (Accutane, Absorica), used for severe acne, affects the oil glands in your eyelids. About 45-60% of users develop dry eyes, and 10-15% get light sensitivity. This isn’t just discomfort - it makes focusing hard, especially when reading or driving at night. Many people think it’s just a side effect they have to live with, but it’s treatable with preservative-free artificial tears or even tiny plugs inserted in the tear ducts.
Other drugs change the shape of your cornea. Amiodarone, used for irregular heart rhythms, builds up in the front layer of your eye in over 70% of long-term users. It creates a swirling pattern on the cornea that scatters light, causing halos and blurry vision. These deposits usually don’t hurt your sight directly, but they’re permanent in two out of three cases - even after you stop the drug.
Then there are drugs that trigger sudden pressure changes inside the eye. Topiramate (Topamax), prescribed for seizures and migraines, can cause acute angle-closure glaucoma in up to 2% of users. This isn’t gradual blurring - it’s sudden, painful, and dangerous. Symptoms include intense eye pain, headache, nausea, and seeing rainbow-colored rings around lights. If you experience this within the first month of starting Topamax, you need emergency care. Left untreated, it can destroy your vision in less than two days.
And don’t forget corticosteroids. Whether you’re taking them as a pill, inhaler, or injection, these powerful anti-inflammatories can raise eye pressure in 30-40% of people with glaucoma. Even in healthy eyes, continuous use for six months or more can cause cataracts - specifically a type called posterior subcapsular cataracts that cloud vision right in the center of your sight. People with diabetes are at especially high risk: their chance of developing steroid-induced cataracts is over three times higher than others.
Medications That Can Damage Your Eyes - And How Often
Not all blurred vision is the same. Some side effects are temporary. Others are silent killers. Here’s a breakdown of the most common offenders and what the data says about their real-world impact.
- Topiramate (Topamax): Causes acute glaucoma in 0.5-2% of users. Symptoms show up fast - within days or weeks. 41% of migraine patients stop taking it because of vision problems.
- Amiodarone (Cordarone): Over 70% of long-term users develop corneal deposits. Optic nerve damage happens in 1-2% of those taking more than 400mg daily for over six months.
- Hydroxychloroquine (Plaquenil): Used for lupus and rheumatoid arthritis. Retinal damage occurs in about 1 in 5,000 patients after five years of use. Once it starts, it’s irreversible in 95% of cases.
- Flomax (tamsulosin): A common prostate medication. Nearly all users (95%) develop a condition called intraoperative floppy iris syndrome during cataract surgery. This makes surgery harder and riskier, even if you stopped the drug months earlier.
- NSAIDs (ibuprofen, naproxen): Daily use for over two years increases the risk of retinal bleeding by 0.3-0.5%. After five years, the chance of developing cataracts rises by 28%.
- Corticosteroids: After six months of daily use, 5-7% of users develop cataracts. Eye pressure spikes can happen in as little as two weeks.
- PDE5 inhibitors (Viagra, Cialis): Rare, but linked to optic nerve damage in about 2.5 cases per 100,000 prescriptions. Most cases involve pre-existing conditions like glaucoma or diabetes.
These numbers might seem small, but when you consider how many people take these drugs, the total adds up fast. And many patients don’t realize the connection until it’s too late.
When Blurred Vision Is an Emergency
Not every case of blurry vision needs a trip to the ER. But some do - and waiting even one day can cost you your sight.
Seek immediate medical help if you have:
- Sudden, severe eye pain along with blurred vision
- Seeing rainbow halos around lights with nausea or headache
- Blurred vision that comes on within hours of starting a new drug
- Loss of peripheral vision (like a curtain coming down over your side vision)
- Double vision that doesn’t go away
These symptoms point to acute angle-closure glaucoma, retinal detachment, or optic nerve inflammation - all time-sensitive emergencies. If you’re on Topamax and get sudden eye pain, don’t wait for your next appointment. Go to the emergency room. The same goes if you’re on Plaquenil and notice a dark spot in your central vision - that’s often the first sign of retinal toxicity.
For most other cases - like mild blurriness after starting a blood pressure pill - give it a few weeks. Your body may adjust. But if it doesn’t improve, or gets worse, talk to your doctor. Don’t assume it’s just aging.
Who’s at Highest Risk?
Some people are far more likely to develop vision problems from medications. Knowing your risk can save your sight.
People with diabetes are at greater risk from almost every drug that affects the eyes. Steroids raise eye pressure faster in diabetics. Plaquenil causes retinal damage more easily. Even dry eyes from Accutane heal slower. If you have diabetes and take any of these medications, you need more frequent eye exams.
Older adults are more vulnerable because their eyes naturally lose resilience. Tear production drops, lens clarity decreases, and blood flow slows. A drug that causes mild blurring in a 30-year-old might cause significant vision loss in a 70-year-old.
People with pre-existing eye conditions - glaucoma, macular degeneration, cataracts - are at higher risk too. Medications that increase eye pressure or reduce blood flow can accelerate damage. If you’ve been told you’re a “steroid responder,” you need to be extra careful with any corticosteroid treatment.
Those taking multiple medications are also at risk. Drug interactions can amplify side effects. For example, taking both a beta-blocker for blood pressure and an anticholinergic for overactive bladder can double the chance of blurred vision from ciliary muscle dysfunction.
What You Should Do - Step by Step
Blurred vision from medication doesn’t have to be a surprise. Here’s how to protect yourself:
- Know your drugs. Read the patient information leaflet. Look for “vision changes,” “blurred vision,” or “eye pain” in the side effects section. If it’s listed, pay attention.
- Get a baseline eye exam. If you’re starting amiodarone, Plaquenil, or long-term steroids, ask your doctor for a full eye check before you begin. This gives you a reference point for future changes.
- Schedule regular monitoring. For Plaquenil: annual eye exams with OCT and visual field tests. For amiodarone: yearly slit-lamp exams. For steroids: check eye pressure every 2-4 weeks if you’re on them long-term.
- Tell your eye doctor what you’re taking. Many patients forget to mention their pills. Your ophthalmologist needs to know about every medication - even over-the-counter ones.
- Speak up about symptoms. If your vision changes, don’t downplay it. Say: “I started this medication last month, and now my vision is blurry.” Don’t wait for your doctor to ask.
- Don’t stop your meds without talking to your doctor. Stopping suddenly can be dangerous. But if you’re having vision problems, your doctor might switch you to a safer alternative.
What’s New in Detection and Prevention
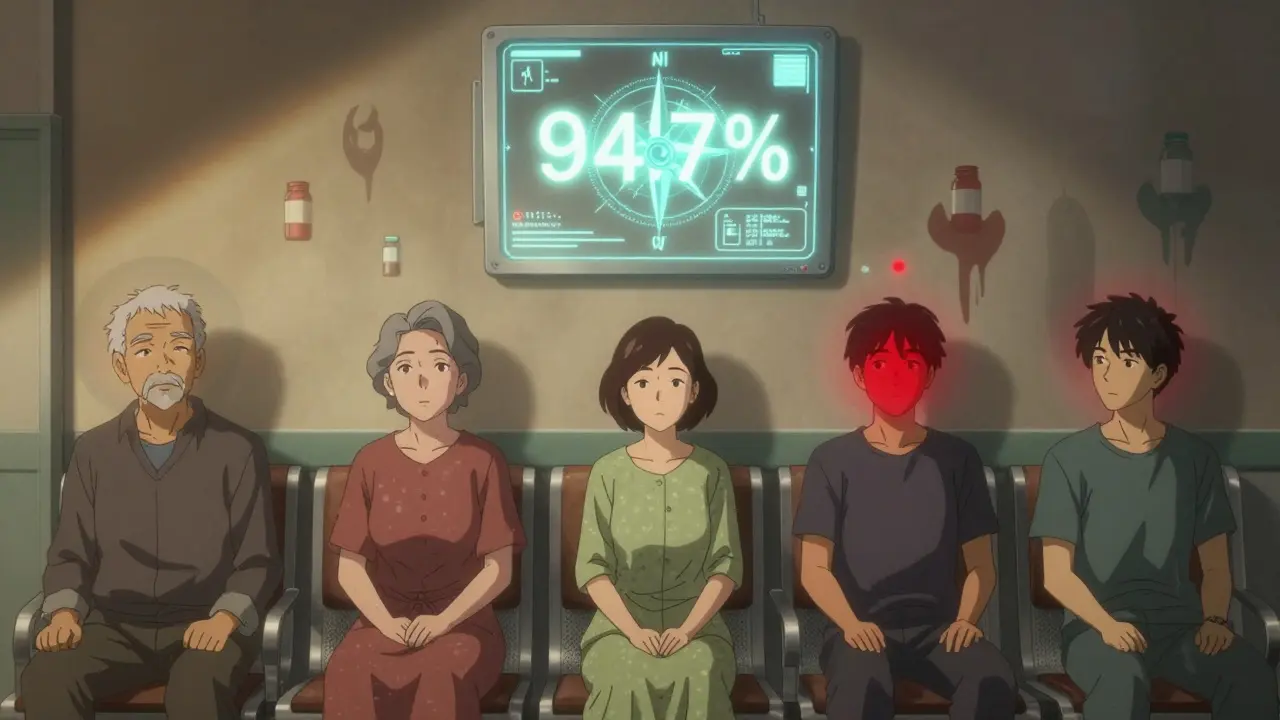
Technology is catching up. In 2023, the FDA approved an AI-powered visual field analyzer called CenterVue’s Compass. It spots early signs of Plaquenil damage with 94.7% accuracy - far better than older methods.
Guidelines have also changed. In early 2024, the American Academy of Ophthalmology lowered the maximum safe dose of Plaquenil from 5.0 mg/kg to 2.3 mg/kg of real body weight. That’s a big shift - and it’s already reducing cases of permanent vision loss.
Hospitals are also stepping up. Nearly 80% of major hospital systems now require an ophthalmology consult before starting high-risk drugs like Plaquenil or amiodarone. That wasn’t common just five years ago.
And the future? Genetic testing may soon identify who’s most likely to develop drug-induced eye damage. Researchers are working on biomarkers that could predict risk before a single pill is taken. Within five years, your doctor might be able to say: “This drug is safe for most people, but your genes make you vulnerable - here’s an alternative.”
Real Stories, Real Consequences
Behind the statistics are people who didn’t get help in time.
On Reddit, a user shared that after six months on Topamax, they developed permanent blurred vision and eye pain. They stopped the drug, but the damage didn’t reverse. Others describe driving at night and seeing halos so bad they couldn’t tell where the road ended.
One woman on Drugs.com said she had cataract surgery and the surgeon had to change his entire approach because she was on Flomax. Her iris flopped around during surgery - something the surgeon wasn’t warned about. She ended up with a detached retina.
These aren’t rare cases. They’re preventable ones.
Your Eyes Are Worth Protecting
Medications save lives. But they can also harm your vision - sometimes silently, sometimes suddenly. The key isn’t avoiding medicine. It’s being informed. If you’re on a drug that lists vision changes as a side effect, don’t ignore blurry vision. Don’t assume it’s just stress or aging. Ask questions. Get checked. Track your symptoms.
Your eyes don’t heal the way your skin or bones do. Once damage is done, it’s often permanent. But with the right awareness and action, you can keep your sight - and keep taking the medications you need to stay healthy.

Diksha Srivastava
January 31, 2026 AT 15:13Just started Plaquenil last month and noticed my vision got a little fuzzy reading small text-was gonna brush it off as screen fatigue, but now I’m scheduling that eye exam ASAP. Thanks for the wake-up call!
Marc Bains
February 1, 2026 AT 17:20As someone who’s lived with diabetes for 20 years, I can’t stress this enough: if you’re on steroids or anything that affects blood sugar, your eyes are the first to scream. I lost 20% of my peripheral vision before I linked it to my prednisone. Get checked. Don’t wait for the ‘it’ll pass’ lie.
Beth Beltway
February 3, 2026 AT 10:10Let’s be real-most people don’t read the tiny print on pill bottles because they’re too lazy to care. Then they blame the doctor when their vision goes sideways. If you’re on Topamax and see rainbows, that’s not ‘side effect,’ that’s a red alert. Stop taking it. Go to the ER. Your eyes aren’t optional.
Lily Steele
February 5, 2026 AT 07:29My mom’s on amiodarone and her eye doc caught the corneal deposits during a routine check. She didn’t have symptoms. Just went in for a refill. That’s why annual scans matter. You don’t need to wait for panic to act.
Gaurav Meena
February 6, 2026 AT 03:30From India, here-so many people skip eye exams because they think ‘if I can see, I’m fine.’ But this post? Game changer. I’m sharing it with my uncle on Flomax. He’s had cataract surgery twice already. No one told him about IFIS. He’s lucky he didn’t go blind.
Eliana Botelho
February 7, 2026 AT 06:04Ugh, another ‘meds are dangerous’ scare piece. I’ve been on Accutane for 8 months and my eyes are dry as a desert-but I just use drops and it’s fine. You’re overhyping this. People are scared of everything now. Also, ‘permanent damage’? Most of these are reversible if caught early. Chill out.
Amy Insalaco
February 8, 2026 AT 18:15While the clinical data presented is superficially compelling, it fails to account for the confounding variable of polypharmacy-induced ocular toxicity. The literature, particularly the 2023 JAMA Ophthalmology meta-analysis, demonstrates that isolated pharmacologic attribution is statistically invalid without controlling for CYP450 enzyme modulation and blood-brain barrier permeability dynamics. Moreover, the FDA’s 2024 Plaquenil dosage revision was based on a cohort with insufficient racial stratification-thus, generalizing these thresholds to non-Caucasian populations constitutes a form of epistemic colonialism in clinical practice.
Shawn Peck
February 10, 2026 AT 11:37Topamax gave me blurry vision and I didn’t know why. Thought I was going crazy. Turned out I had glaucoma in 3 days. Went to ER. Saved my sight. DO NOT IGNORE THIS. I’m alive because I listened. You don’t get a second chance with your eyes.
Russ Kelemen
February 11, 2026 AT 01:58There’s a quiet dignity in taking care of your body when no one’s watching. You don’t need a doctor to tell you something’s off-you just feel it. That’s why this post matters. It’s not about fear. It’s about responsibility. You’re not weak for noticing a change. You’re wise. And if you’re reading this and you’ve been ignoring blurry vision? You’re not alone. But you’re also not powerless. Take the step. Get checked. Your future self will thank you.
Diana Dougan
February 11, 2026 AT 13:14Wow, someone finally wrote a post that’s not just ‘go to the doctor’ but actually tells you what to do. I’m impressed. Also, I just typed ‘corticoesteroids’ instead of ‘corticosteroids’-so yeah, I’m typing this on my phone while eating cereal. But still. This is good. Send it to your grandma.