Stopping benzodiazepines cold turkey can be dangerous. For people who’ve been taking them for months or years, sudden discontinuation can trigger seizures, severe anxiety, hallucinations, or even life-threatening complications. But quitting isn’t the only option-benzodiazepine tapering is the proven, safer way to reduce dependence without risking harm. The good news? Most people can do it successfully with the right plan.
Why Tapering Matters More Than Ever
More than 30 million American adults used benzodiazepines in 2022, and nearly one in five used them long-term. These drugs-like alprazolam (Xanax), lorazepam (Ativan), and clonazepam (Klonopin)-work quickly to calm anxiety or help with sleep. But over time, the brain adapts. What started as a short-term fix becomes a dependency. The body stops making its own calming chemicals, and suddenly, the drug isn’t just helping-it’s holding you together.
That’s why guidelines from the FDA, the Department of Veterans Affairs, and 10 major medical societies now strongly recommend tapering for anyone using benzodiazepines daily for more than a month. The risk isn’t just withdrawal-it’s long-term damage. Older adults face higher chances of falls and memory loss. Veterans with PTSD see worse outcomes when benzos are used long-term. And for anyone with a history of substance use, the risk of relapse spikes.
Abandoning benzos abruptly carries a 20-40% chance of severe withdrawal. Tapering cuts that risk dramatically. But how slow is slow enough? And what does a real, working taper look like?
How Fast Should You Taper?
There’s no universal timeline. A person who took Xanax for three months needs a different plan than someone on Klonopin for five years. The 2024 Joint Clinical Practice Guideline gives clear, evidence-based ranges:
- 2-8 weeks of use → taper over at least 2 weeks
- 8 weeks to 6 months → taper over at least 4 weeks
- 6 months to 1 year → taper over at least 8 weeks
- More than 1 year → taper over 6 to 18 months
For most people, starting with a 5-10% reduction every 2-4 weeks works best. That might sound painfully slow-but rushing leads to setbacks. A 10% drop on a 10mg daily dose of diazepam is just 1mg. On a 2mg dose of alprazolam, it’s 0.2mg. Tiny steps. But they add up.
Some people need even slower tapers. If anxiety spikes, sleep vanishes, or you feel dizzy or electric shocks in your skin (a common withdrawal sign), pause the reduction. Stay at the current dose for another 2-4 weeks. Then try again. Tapering isn’t a race. It’s a process of listening to your body.
The Three Main Tapering Approaches
Not all tapering is the same. There are three proven methods, each with pros and cons.
1. Stay on the Same Medication
This is the simplest approach. You keep taking your current benzo and reduce the dose gradually. Works well if you’re already on a long-acting one like diazepam (Valium) or clonazepam. But if you’re on a short-acting drug like alprazolam (Xanax), withdrawal symptoms can hit harder between doses. That’s why many clinicians recommend switching.
2. Switch to a Longer-Acting Benzo (Diazepam)
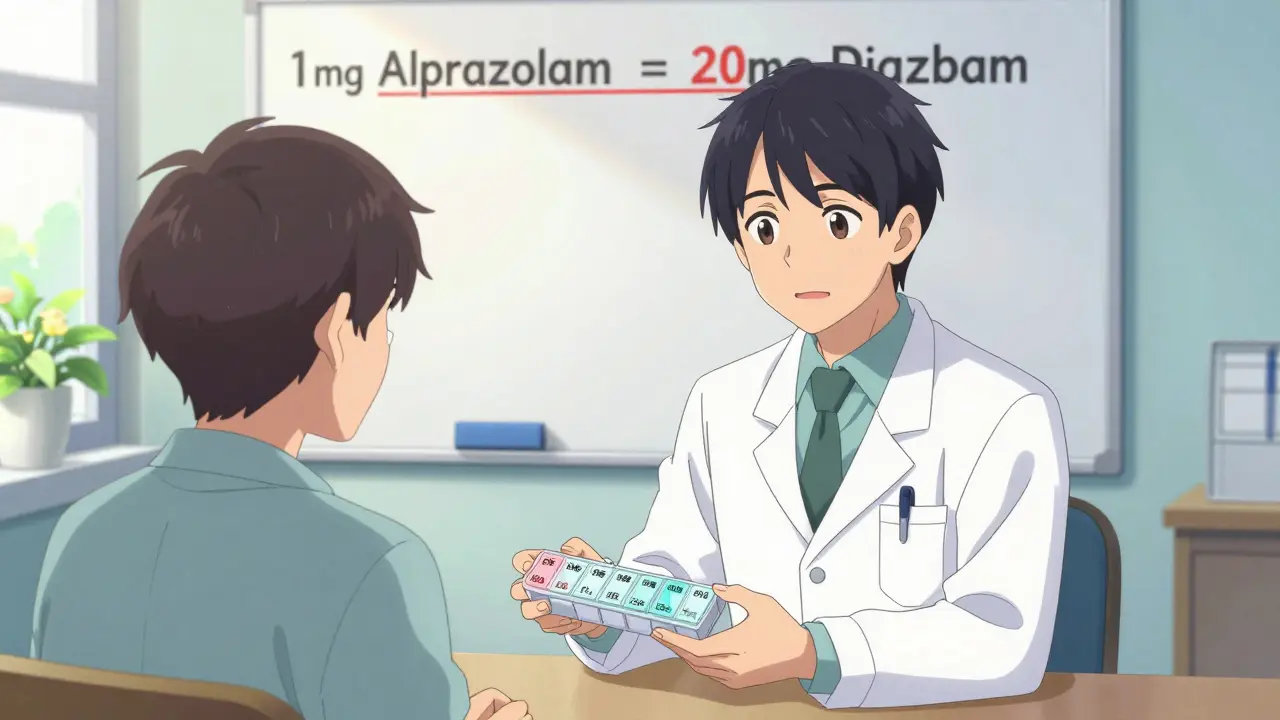
This is the gold standard for most tapers. Diazepam has a half-life of up to 100 hours. That means it stays in your system longer, smoothing out the highs and lows of withdrawal. Switching from alprazolam to diazepam isn’t just a swap-it’s a precise math problem.
1mg of alprazolam = 20mg of diazepam. So if you’re taking 1mg of Xanax daily, you’d start at 20mg of diazepam. Then reduce by 5-10% every 2-4 weeks. This method gives more stable blood levels and fewer withdrawal spikes. It’s why the VA, Oregon Health Authority, and major psychiatric societies all recommend it for complex cases.
3. Use Adjunct Medications
Some people need extra support. Antidepressants like SSRIs can help with underlying anxiety. Sleep aids like trazodone or mirtazapine can replace benzos for insomnia. Beta-blockers may help with heart palpitations. But these aren’t substitutes for tapering-they’re tools to make it bearable.
Don’t use other sedatives like alcohol, melatonin in high doses, or over-the-counter sleep aids without medical supervision. They can interfere or mask symptoms.
Who Should Taper-and Who Shouldn’t
Not everyone needs to stop. If you’ve been on a low dose for a year and it’s helping you function-without side effects-your doctor might say it’s okay to stay on it. But for most people, the risks outweigh the benefits.
Strong reasons to taper:
- You’re over 65 (benzos increase fall risk by 40%)
- You’re on multiple benzodiazepines
- You’ve been using them longer than 6 months
- You have a history of substance use disorder
- You have cognitive decline or traumatic brain injury
- You’re a veteran with PTSD
These groups benefit most from tapering. The VA saw a 23.7% drop in long-term benzo use among veterans between 2020 and 2023 after implementing mandatory tapering protocols. That’s not just numbers-it’s fewer falls, better sleep without drugs, and more control over their lives.
But if you’ve tried every alternative and benzos are the only thing keeping you from panic attacks, your doctor might suggest staying on the lowest effective dose. That’s not failure. It’s harm reduction.
What Happens During Withdrawal?
Withdrawal symptoms vary. Some people feel nothing. Others get hit hard. Common signs include:
- Increased anxiety or panic attacks
- Insomnia or nightmares
- Tremors or muscle twitches
- Sensory changes (tingling, light sensitivity, buzzing sounds)
- Dizziness or vertigo
- Heart palpitations
- Nausea or stomach cramps
These usually peak within 1-2 weeks after a reduction and fade over days. But in some cases, symptoms linger for weeks-this is called protracted withdrawal. It’s rare, but real. The key? Don’t rush back to your old dose. Instead, pause the taper, stabilize, and wait. Most people recover fully.
One study found that when people combined tapering with cognitive behavioral therapy (CBT), 68.3% successfully stopped benzos. Without CBT, that number dropped to 42.1%. Therapy helps rewire the brain’s fear response. It teaches you to sit with anxiety instead of medicating it.

How to Make Tapering Work
Success isn’t just about the dose. It’s about support, structure, and self-care.
- Work with one doctor and one pharmacy. This prevents dose spikes or accidental double prescriptions.
- Get prescriptions for 1-2 weeks at a time. It forces accountability and reduces the chance of misuse.
- Track your symptoms daily. Use a notebook or free app (some are being tested by NIH in 2026). Note mood, sleep, tremors, and anxiety levels.
- Build a support system. Talk to someone who gets it-a therapist, peer support group, or trusted friend.
- Get moving. Even 20 minutes of walking daily reduces withdrawal anxiety.
- Stick to sleep hygiene. No screens before bed. Cool, dark room. Consistent bedtime.
- Avoid caffeine and alcohol. Both worsen anxiety and disrupt sleep during tapering.
Clarity matters. If you’re unsure whether your symptoms are withdrawal or a new problem, call your doctor. Don’t guess. Don’t push through. Tapering is not a solo mission.
The Future of Tapering
Change is happening fast. In 2024, 28 U.S. states now require tapering plans for prescriptions longer than 90 days. The VA has made it policy. The FDA now requires warning labels on all benzodiazepine packaging.
And new tools are coming. The NIH is funding a mobile app that tracks symptoms in real time and suggests dose adjustments based on your data. It’s being tested right now-and early results show it helps people taper more confidently.
By 2026, tapering won’t be an exception. It’ll be standard care. The goal isn’t just to stop the drug-it’s to rebuild a life without it.
When to Seek Help
Call your doctor immediately if you experience:
- Seizures
- Severe hallucinations or delusions
- Extreme confusion or disorientation
- Thoughts of self-harm
These are medical emergencies. Go to the ER or call emergency services. You are not alone. Help is available.

steve rumsford
January 7, 2026 AT 20:22Been on Klonopin for 7 years. Tapered at 5% every 3 weeks. Took 14 months. Felt like dying for the first 6 but now I sleep without pills and my brain doesnt feel like jelly. Worth it.
Anastasia Novak
January 8, 2026 AT 01:48Oh wow. So you’re telling me the VA and FDA finally admitted they spent 30 years gaslighting people into thinking benzos were harmless? The irony is thicker than my Xanax withdrawal brain fog. I’m crying. Not literally. But emotionally. Like, full Shakespearean tragedy vibes.
LALITA KUDIYA
January 8, 2026 AT 20:24thank you for this. i was scared to stop but now i feel hopeful 😊
Poppy Newman
January 9, 2026 AT 11:56Switching to diazepam sounds like a game-changer 🌟 I’ve been on Xanax for 3 years and the withdrawal spikes are brutal. This makes so much sense now. Thanks for breaking it down!
Christine Joy Chicano
January 11, 2026 AT 05:09The 2024 Joint Clinical Practice Guideline’s tapering windows are meticulously evidence-based, and I appreciate how the author contextualized the pharmacokinetics of long- versus short-acting benzodiazepines. The diazepam substitution protocol, in particular, is grounded in neuroadaptive tolerance theory and aligns with the 2023 Cochrane meta-analysis on withdrawal mitigation. Additionally, the emphasis on CBT as a neuroplasticity modulator is not merely adjunctive-it’s foundational to long-term recovery. I’d love to see longitudinal data on neurocognitive recovery post-taper.
Ayodeji Williams
January 11, 2026 AT 18:46you guys are all missing the point. the real problem is the pharmaceutical industry made billions off this. they told doctors benzos were safe then turned around and said 'oh wait no theyre addictive'. they profit from your suffering. they even paid for this 'taper guide'. its all a scam.
Kyle King
January 12, 2026 AT 22:50Wait… so if you taper slowly, you're not really quitting-you're just letting Big Pharma slowly drain your bank account while you 'learn to cope'. The FDA didn't care until 2024 because they're on the payroll. I read a forum post once where a guy said the 'withdrawal symptoms' are just your body trying to detox from the glyphosate in your water. Coincidence? I think not.
Anthony Capunong
January 13, 2026 AT 10:24Why are we letting foreigners dictate our medical standards? The VA’s guidelines are fine, but India and the UK don’t know what real anxiety is. We need American solutions, not European slow-taper nonsense. Just take the damn pill and get over it.
Aparna karwande
January 14, 2026 AT 13:04Oh please. You people are so desperate for a magic fix you’ll swallow any government pamphlet with a fancy logo. Benzodiazepines aren’t the problem-weak willpower is. My grandmother survived the Partition without a single pill, and you’re crying over 0.2mg reductions? Pathetic. You think therapy fixes trauma? Ha. You need discipline, not a mood journal. And don’t even get me started on this ‘diazepam switch’-it’s just a corporate ploy to sell more pills under a different name. Wake up.
And don’t give me that ‘harm reduction’ nonsense. If you can’t handle life without a chemical crutch, maybe you shouldn’t be allowed to drive, vote, or breathe fresh air. This isn’t a medical issue-it’s a moral failure disguised as science.
Look at the VA numbers. 23.7% reduction? That’s because they forced people. No one’s asking for permission to be strong. No one’s asking for a ‘plan’. You just do it. Or you stay broken. Simple.
I’ve seen men in my village in Uttar Pradesh work 18-hour days, bury their dead, raise kids, and never touch a pill. You think they needed a 18-month taper? They needed a spine. And you? You’ve got a smartphone full of self-help apps and a therapist who charges $200/hour to tell you to breathe.
Stop romanticizing weakness. This isn’t a journey. It’s a choice. Choose strength. Or choose the pill. But don’t dress your surrender in clinical jargon and call it ‘evidence-based’.
And yes-I’m Indian. And yes-I’m proud of it. We don’t need your Western guilt trips to tell us what pain is. We lived it. We survived it. We didn’t need a guideline. We needed grit.
Jonathan Larson
January 14, 2026 AT 16:10It is imperative to underscore that the pharmacological discontinuation of benzodiazepines constitutes a neurobiological recalibration process of considerable complexity. The central nervous system, having undergone compensatory downregulation of GABA-A receptor sensitivity, requires a temporally graded reintroduction of endogenous inhibitory tone. Abrupt cessation precipitates a state of hyperexcitability that may manifest in somatic, perceptual, and affective domains, as duly documented in the literature. The recommended tapering protocols, particularly the substitution with long-acting agents such as diazepam, are not merely pragmatic-they are neuroscientifically sound. Furthermore, the integration of cognitive behavioral interventions serves not as an adjunct, but as a necessary coadjutant to restore homeostatic regulation of fear circuitry. The data presented herein reflect not only clinical best practices, but a paradigmatic shift in psychiatric care-from pharmacological dependency to neurobehavioral autonomy. One must approach this transition with the solemnity of a surgical procedure: precise, patient, and profoundly human.
Vince Nairn
January 16, 2026 AT 10:32Wow. So if I'm reading this right, the only thing keeping me from a full mental collapse is a tiny white pill... and now I'm supposed to slowly take away the only thing holding my soul together? Cool. Cool cool cool. Guess I'll just start meditating and eating kale while my brain screams into the void. Thanks for the encouragement.
Emma Addison Thomas
January 16, 2026 AT 21:53Thank you for the clarity. I’ve been tapering for 11 months now and still get the electric zaps-still terrifying. But knowing they’re temporary and not a sign I’m breaking makes all the difference. I’m not ‘weak’ for needing this. I’m healing.
Mina Murray
January 16, 2026 AT 22:48So let me get this straight. You’re telling me the same people who told us SSRIs were ‘safe’ and ‘non-addictive’ are now the ones writing tapering guidelines? And you trust them? The FDA approved alprazolam in 1981. They knew. They’ve always known. This isn’t a ‘new discovery’-it’s damage control. And don’t even get me started on CBT. It’s just a fancy way of telling you to ‘think positive’ while your nervous system is on fire. The real solution? Ban these drugs. Not ‘taper’. Ban them.
Kamlesh Chauhan
January 18, 2026 AT 09:07all this is just so much bs. i took xanax for 2 years and just quit. no taper. no diazepam. no therapy. just stopped. i felt bad for a week and now im fine. why make it so complicated? you people just want to make money off anxiety
Jonathan Larson
January 20, 2026 AT 08:41Your comment raises an important point, but it risks conflating individual resilience with population-level medical safety. While some may successfully discontinue abruptly, the statistical risk of seizure, psychosis, or prolonged withdrawal in long-term users is not trivial. The guidelines exist not to pathologize personal strength, but to prevent preventable harm. The fact that you survived does not invalidate the need for structure in those who do not.