When your heart skips a beat, races too fast, or pounds like it’s trying to escape your chest, it’s not just nerves-it could be an arrhythmia. These aren’t rare quirks. About 1 in 4 adults will develop some form of abnormal heart rhythm by age 80. Three of the most common types-atrial fibrillation, bradycardia, and tachycardia-can sneak up on you, even if you feel fine. But knowing the signs, causes, and real-world treatments can change everything.
What Is Atrial Fibrillation?
Atrial fibrillation, or AFib, is when the upper chambers of your heart (the atria) fire off chaotic electrical signals. Instead of beating in sync, they quiver or flutter. This messes up blood flow, which can lead to clots, strokes, and heart failure over time. The American Heart Association says AFib affects between 2.7 and 6.1 million people in the U.S. alone-and that number is rising with aging populations. In Australia, one in ten people over 75 have it. Many don’t even know they have it until they have a stroke. Symptoms? Not always obvious. Some people feel:- A fluttering or pounding in the chest
- Shortness of breath during light activity
- Fatigue that won’t go away
- Dizziness or lightheadedness
- Heart palpitations that come and go
How Is AFib Diagnosed?
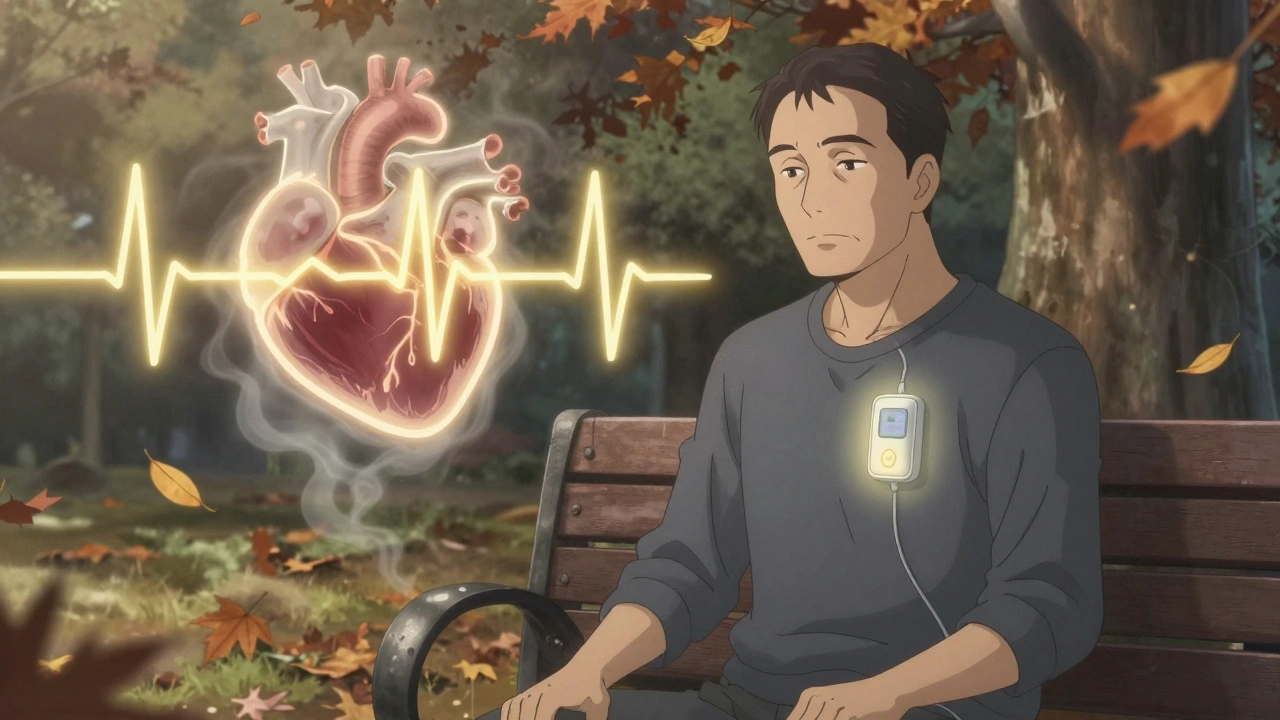
There’s no magic test. Diagnosis starts with your doctor listening to your heart and asking about your history: Do you have high blood pressure? Diabetes? Sleep apnea? Have you been drinking heavily? These all raise your risk. The gold standard is a 12-lead ECG. It’s quick, painless, and shows the exact pattern of your heart’s electrical activity. If your heart rhythm is irregular on the screen, it’s AFib. But sometimes, AFib comes and goes. That’s called paroxysmal AFib. In those cases, doctors may ask you to wear a portable monitor for 24 to 48 hours-or even longer-so they can catch the episode. Some people use smartwatches with ECG features now, but these aren’t replacements for medical-grade devices. An echocardiogram might follow to check your heart’s structure. Blood tests look for thyroid problems or electrolyte imbalances that could be triggering the rhythm issue.How Is AFib Treated?
Treatment isn’t one-size-fits-all. It depends on how long you’ve had it, your symptoms, and your stroke risk. Rate control is the first step for most people. The goal isn’t to make your heart beat normally-it’s to slow it down enough so you don’t feel awful. Medications like beta-blockers (metoprolol), calcium channel blockers (diltiazem), or digoxin help with this. Rhythm control tries to restore a normal heartbeat. This might mean drugs like amiodarone or flecainide. Or it could mean a procedure called cardioversion-a controlled electric shock that resets your heart. It’s done under light sedation and works well for recent-onset AFib. But if drugs don’t work, or if you’re young and active and tired of feeling off, ablation is an option. This procedure uses heat or cold to scar small areas of heart tissue that are sending wrong signals. Newer techniques like pulsed field ablation use electric pulses instead of extreme temperatures, reducing damage to nearby tissues and lowering complications. For high-risk patients-especially those over 65 with other conditions-anticoagulants like apixaban or rivaroxaban are critical. They prevent clots from forming. Warfarin is still used, but it needs frequent blood tests. Newer drugs don’t.What Is Bradycardia?
Bradycardia means your heart beats slower than 60 times per minute. Sounds bad? Not always. Athletes and very fit people often have resting heart rates of 40-50 bpm. That’s normal. Their hearts are strong-they pump more blood per beat, so they don’t need to beat as often. But if you’re not an athlete and your heart is beating too slowly, you might feel dizzy, tired, or faint. You might struggle to climb stairs. In severe cases, your brain doesn’t get enough oxygen, leading to blackouts. Causes include:- Aging of the heart’s natural pacemaker (the sinoatrial node)
- Heart disease or heart attacks
- Electrolyte imbalances (low potassium or calcium)
- Underactive thyroid
- Medications like beta-blockers or digoxin
How Is Bradycardia Diagnosed and Treated?
Same as AFib: start with an ECG. If your heart rate is low and you have symptoms, doctors will look for underlying causes. Blood tests check thyroid and electrolytes. A stress test might be done to see if your heart rate rises properly during activity. If it’s harmless-like in a marathon runner-no treatment is needed. If it’s dangerous, the fix is often a pacemaker. It’s a small device implanted under the skin near the collarbone. Wires connect to your heart and deliver tiny electrical pulses when your heart rate drops too low. Modern pacemakers adjust automatically-you can still run, swim, or lift weights with one. Some people with bradycardia also have AFib. That’s called tachy-brady syndrome. It’s tricky to treat because drugs that slow the fast beats can make the slow ones worse. Pacemakers help balance it out.What Is Tachycardia?
Tachycardia means your heart beats faster than 100 beats per minute at rest. It’s not a single condition-it’s a category. There are two main types:- Supraventricular tachycardia (SVT): Starts above the ventricles. Common in younger people. Often feels like a sudden racing heart, maybe with chest tightness or nausea. Episodes can last seconds or hours.
- Ventricular tachycardia (VT): Starts in the lower chambers. More dangerous. Can lead to cardiac arrest if not treated. Often linked to heart damage from past heart attacks or cardiomyopathy.
- Sudden, pounding heartbeat
- Chest pain or pressure
- Shortness of breath
- Feeling like you’re going to pass out
- Sweating or anxiety
How Is Tachycardia Diagnosed and Treated?
ECG is the first step. But because episodes can be brief, doctors often use portable monitors or event recorders. For SVT, a simple trick called the Valsalva maneuver can sometimes stop it. It’s when you hold your breath and bear down like you’re having a bowel movement. It stimulates the vagus nerve and can reset the rhythm. Medications like adenosine can be given in the ER to stop an episode. For recurring SVT, ablation is highly effective-curing it in 90% of cases. VT is treated differently. If it’s causing symptoms or you’ve had a heart attack, you might need an implantable cardioverter-defibrillator (ICD). It’s like a pacemaker but can deliver a strong shock if your heart goes into a deadly rhythm. Lifestyle changes matter too: cutting caffeine, managing stress, avoiding alcohol, and treating sleep apnea can reduce episodes.
Why Do These Arrhythmias Matter?
AFib increases your stroke risk five times. Bradycardia can cause falls and injuries from fainting. Tachycardia can lead to heart muscle damage over time. But here’s the good news: all three are manageable. Many people live full, active lives with these conditions-especially when caught early. The key is awareness. If you feel your heart acting strange-racing, skipping, or pounding without reason-don’t ignore it. Write down when it happens, how long it lasts, and what you were doing. That info helps doctors more than any test.What Can You Do Right Now?
You don’t need to wait for symptoms to get worse. Here’s what to try:- Check your pulse weekly. Use your fingers on your wrist or neck. Is it steady or irregular?
- Limit alcohol. Even one drink a day can trigger AFib in some people.
- Control blood pressure. High BP is the #1 risk factor for AFib.
- Get enough sleep. Sleep apnea is strongly linked to arrhythmias.
- Stay active. Walking 30 minutes a day lowers your risk of all three types.
- Know your family history. Arrhythmias can run in families.
Can arrhythmias go away on their own?
Sometimes, yes. Brief episodes of SVT or paroxysmal AFib can resolve without treatment. But if you’ve had more than one episode, or if you’re over 60, it’s unlikely to disappear permanently. Even if symptoms fade, the underlying risk-like stroke from AFib-doesn’t. That’s why medical evaluation is still needed.
Is it safe to exercise with an arrhythmia?
Usually, yes-but it depends. People with well-controlled AFib or SVT can often exercise safely, even at moderate intensity. Those with ventricular tachycardia or severe bradycardia need clearance from a cardiologist. Avoid extreme heat, dehydration, and caffeine before workouts. Always listen to your body: if you feel dizzy or chest pain, stop and get help.
Do I need to take blood thinners for life if I have AFib?
Not always. Doctors use a scoring system (like CHA₂DS₂-VASc) to estimate your stroke risk. If your score is low, you might not need them. But if you’re over 65, have high blood pressure, diabetes, or heart failure, long-term anticoagulants are usually recommended. Stopping them without medical advice increases stroke risk dramatically.
Can stress cause arrhythmias?
Stress doesn’t cause arrhythmias directly, but it can trigger them in people who are already at risk. High stress raises adrenaline, which can push a sensitive heart into AFib or SVT. Chronic stress also raises blood pressure and inflammation-both risk factors. Managing stress with sleep, breathing exercises, or therapy can reduce episodes.
Are smartwatches reliable for detecting arrhythmias?
They can be helpful for spotting irregular rhythms, especially AFib. Apple Watch and Fitbit models with ECG features have FDA clearance for this. But they’re not diagnostic tools. They can give false positives or miss episodes. If your watch alerts you, follow up with a doctor and get a proper ECG. Don’t rely on it alone.
Sandridge Nelia
December 4, 2025 AT 07:19I’ve been using my Apple Watch to track my pulse since my last checkup, and it flagged an irregular rhythm once. I didn’t panic, but I scheduled an ECG and turns out it was paroxysmal AFib. So glad I didn’t ignore it. These days I check my pulse every Sunday morning - simple, free, and life-saving.
Also, if you’re over 65, ask your doc about AFib screening. My grandma got hers done at the community clinic and they caught it before she had a stroke. Life changed for her - in a good way.
Mark Gallagher
December 6, 2025 AT 04:44Let’s be clear: if you’re not getting a 12-lead ECG every time you feel your heart skip, you’re doing it wrong. Smartwatches are toys for people who don’t understand cardiac physiology. The FDA doesn’t clear them for diagnosis - they’re glorified pedometers with a fancy algorithm. And if you think caffeine is the culprit, you’re ignoring the real problem: poor lifestyle discipline.
Wendy Chiridza
December 6, 2025 AT 22:49I had SVT when I was in my 30s and the Valsalva maneuver worked like magic every time. No meds, no hospital visits. I still teach it to my yoga students now. Just breathe in deep, pinch your nose, bear down like you’re pushing out a baby, and hold for 10 seconds. It’s wild how something so simple can reset your heart.
Also, sleep apnea is the silent killer here. If you snore, get tested. It’s not just about tiredness - it’s about your heart.
Pamela Mae Ibabao
December 8, 2025 AT 19:27Oh honey, I used to think my heart was just being dramatic until I fainted in the grocery store. Turns out I had tachy-brady syndrome - my heart would race then drop to 38 bpm. My cardiologist said I was lucky I didn’t hit my head. Now I’ve got a pacemaker and I’m back to hiking, dancing, and yelling at my cats like normal.
Don’t let anyone tell you aging means you have to suffer. You deserve to feel good. And yes, I cry when I think about how close I came to not being here. But I’m here. And I’m grateful.
Also, I love my pacemaker. It’s like a tiny superhero in my chest. 🤍
Gerald Nauschnegg
December 10, 2025 AT 18:10Guys I just got back from my electrophysiologist and they said my AFib is paroxysmal and I’m a candidate for pulsed field ablation. I was skeptical but they showed me the data - 90% success rate, way less damage than old-school ablation. I’m getting it next month. If you’re tired of feeling like your heart’s a broken drum, this is your sign to ask your doc about it. No more beta-blockers making me feel like a zombie.
Also, I’m 52 and I walk 5 miles a day. That’s how I stay out of the hospital. Don’t wait till you’re 70 to start moving.
Palanivelu Sivanathan
December 11, 2025 AT 18:09My brother died at 48 from a stroke caused by undiagnosed AFib!!! He was healthy!!! He ate kale!!! He meditated!!! And yet his heart betrayed him!!!
Do you know what the real enemy is??? It’s the pharmaceutical industry!!! They want you on blood thinners forever!!! They profit from your fear!!!
My cousin in Kerala cured his arrhythmia with turmeric tea and chanting mantras!!! Why are we ignoring ancient wisdom???
And why does no one talk about EMF radiation from cell phones??? It’s scrambling our heart’s electrical signals!!!
I’m not saying don’t go to the doctor… I’m saying question everything!!!
Wake up!!!
Joanne Rencher
December 12, 2025 AT 01:57I read this whole thing and honestly? It’s just a long ad for cardiology clinics. Everyone’s got a heart that skips sometimes. You’re not special. Stop Googling symptoms and go for a walk. Also, why does every article now need to be 2000 words long? Just tell me what to do.
Also, I don’t need a pacemaker. I need a better life.
Erik van Hees
December 12, 2025 AT 16:51Let me break this down for you. Bradycardia in athletes? Totally normal. But if you’re a 60-year-old who hasn’t moved since 2012 and your heart’s at 52 bpm? That’s not ‘normal’ - that’s your body screaming for help. Same with AFib - if you’re drinking wine every night and your pulse is irregular, it’s not ‘just stress.’ It’s alcohol-induced cardiomyopathy waiting to happen.
And if you think smartwatches are diagnostic tools, you’re the reason ERs are packed. I’ve seen 3 people come in because their Fitbit said ‘possible AFib’ - turns out they were just nervous. But the damage? They’re now on blood thinners for no reason.
Get an ECG. Not a watch. Not a YouTube video. An ECG.
Cristy Magdalena
December 13, 2025 AT 11:38I didn’t know I had AFib until I passed out at my daughter’s graduation. I was so embarrassed. But then I found out I’d been having silent episodes for years. I felt so guilty - like I’d been neglecting myself. Like I’d been ignoring the whispers my body was giving me.
Now I take my pills. I check my pulse. I cry sometimes when I think about how close I came to not seeing her walk across that stage.
It’s not just about medicine. It’s about love. You owe it to the people who love you to listen to your body. Even when it’s quiet.
Even when it’s scary.
Even when you’re tired.
I’m still here. And I’m trying.
And that’s enough.
Adrianna Alfano
December 14, 2025 AT 22:59My abuela had AFib and she’d always say ‘mi corazon baila’ - my heart dances. I thought she was being poetic until I saw her ECG. She had the most chaotic rhythm you’ve ever seen. But she danced every Sunday. Made tamales. Sang rancheras. She didn’t let it define her.
My mom’s on apixaban now. She hates the pills but she takes them. We don’t talk about it much. But I hold her hand when she checks her pulse. That’s our thing now.
Heart stuff isn’t just clinical. It’s family. It’s legacy. It’s the quiet moments when you notice someone’s breathing different.
And yeah, I misspelled ‘rancheras.’ Sorry. But I meant it.
Casey Lyn Keller
December 15, 2025 AT 20:15Look, I’ve read every study on this. The whole arrhythmia narrative is controlled by big pharma and the device manufacturers. Pacemakers? $50k each. Ablations? $100k. Blood thinners? Lifetime prescriptions. Who benefits?
Meanwhile, the real causes - toxins, mold, chronic inflammation - are ignored. And don’t get me started on the 5G towers near hospitals.
My uncle had a pacemaker and died 6 months later. The doctors said ‘natural causes.’ I say it was the device. They don’t want you to know this.
Don’t trust the system. Trust your gut. And stop letting them scare you into surgery.
Mindy Bilotta
December 15, 2025 AT 22:33My mom got a pacemaker last year and now she’s back to gardening and playing with her grandkids. I used to think they were scary - all wires and beeps. But the modern ones? Tiny. Quiet. Smart. She says it’s like having a little heart coach in her chest.
Also, if you’re Canadian, get your pulse checked at your pharmacy. They do it for free. No appointment. Just walk in. I did it last month - turns out my resting rate was 58, which is fine. But I didn’t know until I checked.
Small steps. Big difference.