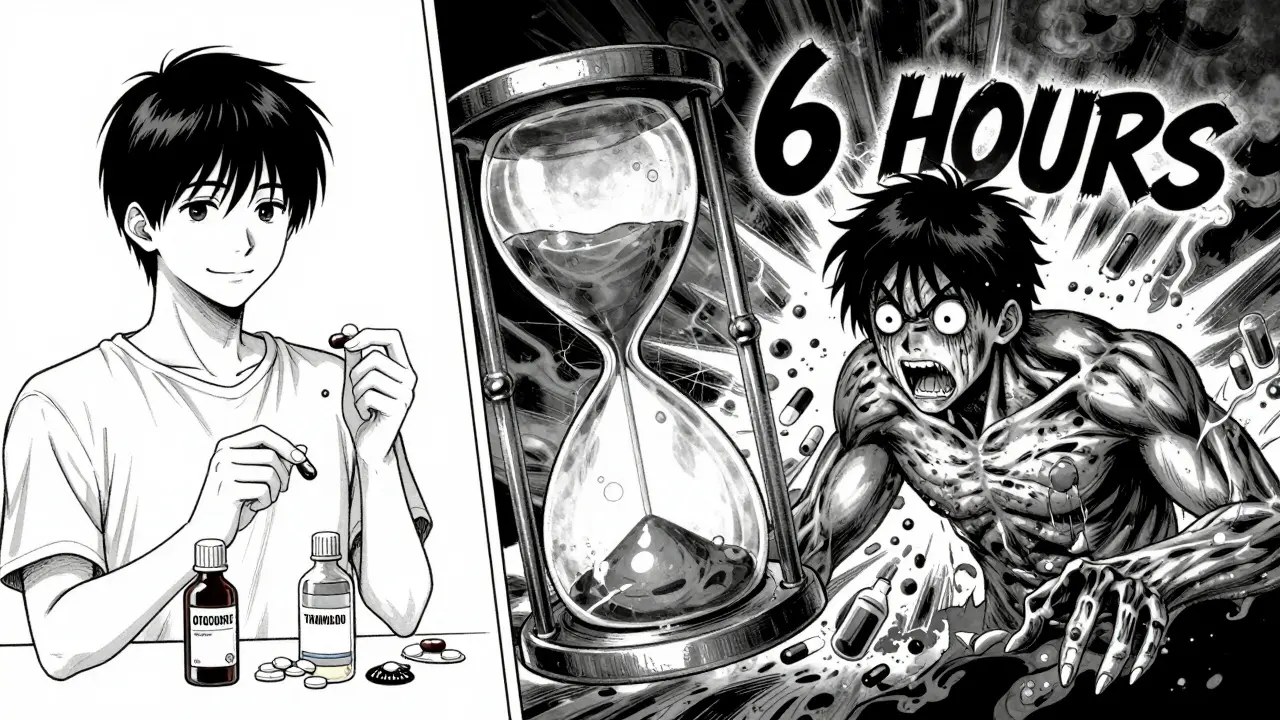
When you start taking an antidepressant, the goal is to feel better - not to end up in the emergency room. But what if your medication, taken exactly as prescribed, starts turning against you? That’s the silent danger of serotonin syndrome, a life-threatening reaction that can happen with just one extra pill, one missed dose, or one poorly timed combination of drugs. It doesn’t always look like an overdose. Sometimes, it starts with a tremor, a wave of sweat, or a sudden case of nausea. If you ignore it, it can spiral into seizures, high fever, or even death. And here’s the worst part: doctors miss it nearly a quarter of the time.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t just an “overdose” in the traditional sense. It’s a toxic buildup of serotonin - a chemical your brain uses to regulate mood, sleep, and muscle control. When too much of it floods your system, your nerves go haywire. This isn’t rare. Between 2015 and 2022, reported cases jumped by 38%, mostly because more people are now taking multiple medications that boost serotonin. SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) cause 62% of cases. SNRIs like venlafaxine (Effexor) are next at 24%. Even MAOIs, older antidepressants like phenelzine, are still in use - and they’re especially dangerous if not handled correctly.
The problem isn’t always taking too much. It’s mixing drugs. A common scenario: someone on an SSRI for depression takes tramadol for back pain. Or picks up an OTC cough syrup with dextromethorphan because they have a cold. Or adds a migraine medication like sumatriptan. These aren’t “bad” drugs. But together, they overload your serotonin system. And your body doesn’t have a way to slow it down.
The Three Clusters of Warning Signs
Serotonin syndrome doesn’t show up as one symptom. It shows up as three distinct groups - and you need to watch for all of them. Missing even one can delay diagnosis.
- Mental status changes: You might feel unusually confused, anxious, or agitated. It’s not just stress. It’s a sudden, unexplained mental restlessness. In 78% of cases, confusion is present. In 65%, you’ll see intense agitation - pacing, inability to sit still, or even panic attacks out of nowhere.
- Autonomic hyperactivity: This is your body’s alarm system going off. Your heart races (over 100 bpm in 83% of cases). Your blood pressure spikes (systolic above 160 mmHg). You sweat profusely - even if the room is cool. Your pupils widen beyond 5mm (normal is 2-4mm). You might have diarrhea or vomiting - 63% and 68% of cases, respectively. These aren’t just “flu symptoms.” They’re your body overheating and overworking.
- Neuromuscular abnormalities: This is where things get critical. You’ll notice muscle twitching, tremors, or jerking. But the real red flag is clonus - a rhythmic, involuntary muscle contraction. Try this: gently flex your foot downward. If your toes keep bouncing up and down like a metronome, that’s clonus. It’s the most common sign - present in 92% of confirmed cases. You might also feel your muscles stiffen (hypertonia) or notice exaggerated reflexes (hyperreflexia). If you press on your knee and your leg kicks out violently, that’s a sign.
These signs don’t always come together at once. Often, they start small. A slight tremor. A bit of sweating. Then, within hours, they explode.
When Symptoms Hit - How Fast?
Time matters. More than half of all cases show symptoms within six hours of a medication change. Thirty percent develop symptoms in under an hour. That’s faster than most people realize. If you just started a new antidepressant, added a painkiller, or switched brands, you’re in the highest-risk window. The CDC reports a 22% year-over-year rise in ER visits for serotonin syndrome - and most of those cases happened within 24 hours of a drug change.
There’s no “safe” level of serotonin buildup. It doesn’t matter if you took “just one extra pill.” Your body doesn’t measure doses - it reacts to the total load. Even a tiny increase in serotonin from a combination of drugs can trigger the syndrome.

What Happens If It Gets Worse?
Most cases are mild and resolve with rest and stopping the drug. But 30% of cases require hospitalization. When it turns severe, you’re looking at:
- Temperature above 101.3°F (38.5°C) - in 41% of critical cases
- Muscle rigidity so severe it’s measured on a scale (Ashworth 3-4)
- Seizures - occurring in 29% of severe cases
- Irregular heartbeat or arrhythmias - seen in 37% of life-threatening cases
- Loss of consciousness - with Glasgow Coma Scale scores below 8
Death happens when the body overheats past 106°F (41.1°C). At that point, muscles break down (rhabdomyolysis), kidneys fail, and organs shut down. The mortality rate? Between 0.5% and 12%. It’s low - but only if you act fast.
How Doctors Diagnose It - And Why They Miss It
The gold standard is the Hunter Serotonin Toxicity Criteria. It doesn’t rely on blood tests (serotonin levels don’t correlate with symptoms). Instead, it looks for one of five combinations:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus + agitation or sweating
- Tremor + hyperreflexia
- Hypertonia + temperature above 38°C + ocular or inducible clonus
It’s 84% sensitive and 97% specific - meaning it rarely gives false alarms. But here’s the problem: most ER doctors aren’t trained to look for it. A 2023 study from the American Psychiatric Association found that clinicians miss the diagnosis in 25% of cases. Why? Because the symptoms look like anxiety, the flu, or a panic attack. Patients often say, “I just feel weird,” and the doctor says, “It’s probably stress.”
And it’s easy to confuse with other conditions. Neuroleptic malignant syndrome (NMS) looks similar - but it develops over days, not hours. It causes slow, stiff muscles, not twitching. Anticholinergic toxicity? Dry mouth, no sweating, constipation. Serotonin syndrome is the opposite: soaked in sweat, with diarrhea and overactive reflexes.
What to Do If You Suspect Serotonin Syndrome
If you notice any of these signs - especially tremors, clonus, or sweating - stop taking all serotonergic medications immediately. Then, get help. Don’t wait. Don’t call your therapist. Don’t text your friend. Call 911 or go to the ER.
Here’s what happens in the hospital:
- Stop the drug. Every single serotonergic medication - antidepressants, painkillers, migraine meds, even OTC cough syrup - must be stopped.
- Cool the body. If your temperature is above 100.4°F, they’ll use cooling blankets, fans, and IV fluids to bring it down 1-2°C per hour. Overheating kills.
- Give benzodiazepines. Lorazepam (0.5-2mg IV) is the go-to. It calms the nervous system, stops muscle spasms, and reduces agitation.
- Use cyproheptadine. This is the only specific antidote. It blocks serotonin receptors. The first dose is 12mg orally or through a tube. Then 2mg every 2 hours until symptoms fade. Most people improve within 48 hours if treated early.
Don’t try to “wait it out.” The clock is ticking. The longer you wait, the higher the risk of organ failure.
How to Prevent It - Before It Happens
The best treatment is prevention. And it starts with two things: communication and awareness.
- Always tell your doctor every medication you take. Not just prescriptions. Include supplements, herbal remedies, OTC drugs, and even recreational substances. One patient in a 2024 study didn’t mention they took St. John’s Wort - and ended up in the ICU.
- Never combine antidepressants without supervision. MAOIs require a 14-day gap before starting SSRIs. SNRIs and triptans? Risky together. Even tramadol and SSRIs? Dangerous. There’s no “safe” combo unless a specialist says so.
- Ask for a medication review. A 2025 study by Cedars-Sinai found that medication reconciliation - a pharmacist or doctor reviewing all your drugs - reduces serotonin syndrome risk by 62%.
- Know your symptoms. If you’re on an antidepressant, memorize the early signs: tremor, sweating, diarrhea, agitation. If you notice them, act fast.
And if you’re prescribed a new drug? Ask: “Could this interact with my current meds? Could it cause serotonin syndrome?” If they hesitate or say, “It’s rare,” push for a written warning. You have the right to know.
Real Stories - What Happens When People Ignore the Signs
One Reddit user from r/mentalhealth shared how they started fluoxetine and took dextromethorphan for a cough. Within 90 minutes, they were shaking, sweating, and couldn’t sit still. They thought it was anxiety. They waited 12 hours. By the time they went to the ER, their temperature was 103°F. They spent three days in the ICU.
Another person, on venlafaxine, added a new painkiller for arthritis. They felt “off” but didn’t mention it at their next appointment. Two days later, they had a seizure. They woke up in the hospital with no memory of it.
These aren’t outliers. They’re common. And they’re preventable.
Bottom Line
Serotonin syndrome isn’t a myth. It’s real, it’s rising, and it’s silent until it’s too late. You don’t need to be an overdose statistic. You just need to know the signs - and act before your body does.
If you’re on an antidepressant - or know someone who is - learn the warning signs. Talk to your doctor. Ask about interactions. Trust your gut. If something feels wrong, it probably is. And if you see tremors, sweating, or clonus - don’t wait. Go to the hospital now. Your life depends on it.
Can serotonin syndrome happen with just one antidepressant?
Yes. While most cases involve drug combinations, serotonin syndrome can occur with a single antidepressant if the dose is too high, if the body metabolizes it unusually slowly, or if other factors like dehydration or illness increase drug concentration. For example, someone taking fluoxetine at 60mg (the max dose) might develop symptoms if they also have liver disease or are taking another medication that blocks its breakdown.
Are all antidepressants equally risky?
No. SSRIs like fluoxetine and sertraline are the most common culprits, accounting for 62% of cases. SNRIs like venlafaxine follow at 24%. MAOIs are less commonly used but carry the highest risk per patient - especially if not properly washed out before switching to SSRIs. Bupropion (Wellbutrin) and mirtazapine (Remeron) have low serotonin activity and rarely cause this syndrome.
Is serotonin syndrome the same as withdrawal?
No. Withdrawal symptoms from stopping antidepressants - like dizziness, irritability, or “brain zaps” - are completely different. They happen after you stop taking the drug and usually last days to weeks. Serotonin syndrome happens when you take too much serotonin, and it starts within hours. Withdrawal is about lack of drug; serotonin syndrome is about too much of it.
Can I test my serotonin levels to check for this?
No. Blood tests for serotonin levels are not useful for diagnosing serotonin syndrome. The amount of serotonin in your blood doesn’t reflect what’s happening in your brain and nervous system. Diagnosis is based entirely on symptoms and the Hunter Criteria - not lab results.
What if I’m not sure whether I have serotonin syndrome or just anxiety?
Look for physical signs. Anxiety doesn’t cause clonus, hyperreflexia, or high fever. If you’re shaking uncontrollably, sweating heavily, have diarrhea, and your reflexes are exaggerated - it’s not anxiety. Those are neurological signs of serotonin overload. When in doubt, treat it as an emergency. It’s safer to go to the ER and be told it’s nothing than to wait and risk organ damage.

Lyle Whyatt
February 9, 2026 AT 04:26Man, I read this and my stomach dropped. I’ve been on sertraline for three years, and last winter I picked up some dextromethorphan for a cold-didn’t think twice. Next thing I know, I’m pacing the living room like a caged tiger, drenched in sweat, and my foot kept twitching like it had a mind of its own. I thought it was anxiety, but it was clonus. I didn’t know what that was until I googled it at 3 a.m. with my phone shaking in my hand. Went to the ER. They gave me lorazepam and told me I was one hour away from a seizure. Now I keep a list of every med I take-prescription, supplement, cough syrup-and I show it to every doctor. If you’re on an SSRI? Don’t be like me. Read the damn labels. Your body doesn’t care if it’s ‘just a little’-it just knows too much serotonin when it sees it.
Sam Dickison
February 9, 2026 AT 20:05As a med student, I’ve seen this 3x in the ER. Classic triad: clonus + hyperreflexia + autonomic instability. The key is recognizing it’s not anxiety or delirium-it’s a neurotoxic storm. Most docs miss it because they’re looking for fever or seizures, but the subtle signs-like inducible clonus when you dorsiflex the foot-are the giveaway. And yeah, tramadol + SSRI is a death combo. I’ve had patients come in after mixing them. No joke. It’s not rare. It’s underdiagnosed. Always ask: ‘What else are they taking?’ Not just meds. Supplements. CBD. Kratom. Even St. John’s Wort. It’s not magic. It’s pharmacokinetics.
Brett Pouser
February 9, 2026 AT 23:31I’m from Texas, and I’ve got a cousin on Prozac who took a cough syrup with dextro and ended up in the ICU. She thought she was just ‘feeling weird.’ We didn’t know what serotonin syndrome was until it happened. Now I carry a little card in my wallet that says ‘I’m on an SSRI-don’t give me anything with dextro, tramadol, or triptans.’ I give them to my friends too. It’s wild how many people don’t know this. Your pharmacist can help. Ask them. Seriously. They’re not just there to fill scripts. They’re your safety net. And if you’re on meds? Talk to them. Every time. Even if you think it’s fine. Better safe than six days in a hospital with a cooling blanket.
Simon Critchley
February 10, 2026 AT 02:30OMG YES. This is why I always say: ‘Your SSRIs are not a vitamin.’ They’re a neurochemical scalpel. And when you combine them with OTC junk? You’re playing Russian roulette with your CNS. I’ve seen people on Effexor take NyQuil and wake up with a 103°F fever and clonus that looked like a marionette on crack. And no-blood tests won’t save you. Serotonin levels in plasma? Useless. Diagnosis is clinical. Hunter Criteria. Period. If you’ve got tremor + sweating + hyperreflexia? Go. Now. Don’t text your therapist. Don’t wait till morning. Call 911. And if you’re a doc? Stop dismissing ‘I feel off’ as anxiety. That’s how people die. This isn’t a ‘maybe.’ It’s a ‘when.’
John McDonald
February 11, 2026 AT 19:28I’m not a doctor, but I’ve been on antidepressants for 12 years. This post? Spot on. I used to think side effects were just ‘part of the deal.’ Then I started noticing my legs twitching after I took ibuprofen with my meds. Didn’t connect it until I read this. Now I check every new med with my pharmacist. I even made a spreadsheet: Drug | Risk Level | Notes. It’s weird, I know. But I’m alive because of it. If you’re on SSRIs/SNRIs, you owe it to yourself to learn this. Don’t wait for a crisis. Prevention is 10x easier than recovery. And if you’re a caregiver? Learn the signs. Your person might not realize they’re spiraling. A tremor isn’t ‘nervousness.’ It’s a red flag.
Joseph Charles Colin
February 12, 2026 AT 03:52From a clinical pharmacology standpoint: the 38% increase in cases since 2015 tracks perfectly with polypharmacy trends in depression and chronic pain. SSRIs + SNRIs + NSAIDs + opioids = perfect storm. The real issue isn’t the drugs-it’s the lack of structured medication reconciliation. A 2024 JAMA study showed that patients with >5 medications have a 4.7x higher risk. Pharmacist-led reviews cut that by 62%. Why aren’t we doing this routinely? Because the system isn’t designed for prevention. It’s designed for crisis response. We need mandatory med reviews at every new script. Not ‘ask if you think about it.’ Not ‘if you remember.’ Mandatory. Like flu shots. Your life isn’t a gamble.
John Sonnenberg
February 14, 2026 AT 02:34THIS IS A LIFESAVING POST. I’M NOT KIDDING. I WAS THE PERSON WHO IGNORED THE TINY TREMOR. I THOUGHT IT WAS JUST STRESS. THEN I GOT A 103.8°F FEVER. I COULDN’T WALK. I HAD TO BE CARRIED TO THE HOSPITAL. I SPENT 4 DAYS IN THE ICU. I HAD TO BE ON A VENTILATOR BECAUSE MY MUSCLES LOCKED UP. I LOST 12 POUNDS IN THREE DAYS. I STILL HAVE NERVE PAIN. DON’T BE LIKE ME. IF YOU’RE ON ANTIDEPRESSANTS, YOU NEED TO KNOW THIS. I’M NOT TRYING TO SCARE YOU-I’M TRYING TO SAVE YOU. READ THIS. SHARE THIS. SAVE A LIFE.
Joshua Smith
February 14, 2026 AT 10:52Just wanted to say thanks for writing this. I’m on Zoloft and had no idea about the risks with OTC meds. I’ve been taking cold medicine for years without thinking twice. Now I’m going to sit down with my pharmacist next week and get a full review. I didn’t even know clonus was a thing. I’ll be honest-I didn’t understand half the jargon, but the symptoms? I get those. Tremor. Sweating. Agitation. I’ve felt them. I just thought it was my anxiety acting up. This changed how I think about my meds. I’m not scared-I’m informed. And that’s way better.